Transcutaneous electrical nerve stimulation and cryotherapy in the treatment of students with primary dysmenorrhea: pilot study
Main Article Content
Abstract
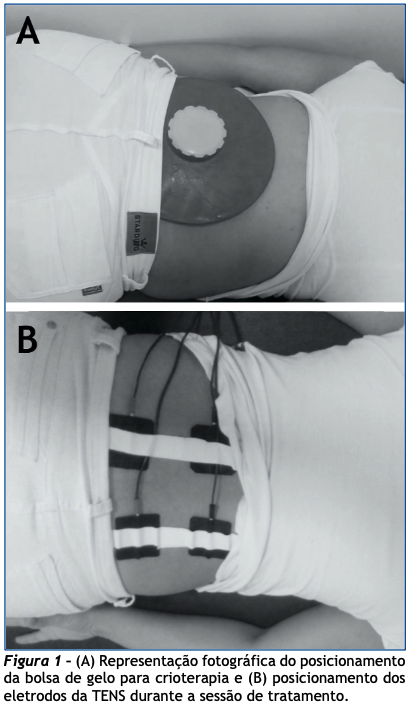
Objective: To compare the effects of Transcutaneous Electrical Nerve Stimulation (TENS) and cryotherapy in relieving painful symptoms in students with primary dysmenorrhea (PD). Methods: Cross-sectional and quantitative study, with 20 university women randomly divided into two groups: TENS Group (GT) whose participants were submitted to a 45 min TENS session with a frequency of 120 Hz and a pulse duration of 100 µs and Cryotherapy Group (CG), whose participants were submitted to a cryotherapy session for 20 min. Women with regular menstrual cycles, nulligravidas, without a report of pelvic disease, and with dysmenorrhea with pain levels between 4 and 10 during the first three days of menstruation were included. Those with contraindications to TENS or cryotherapy and who used drugs up to 24 h before the intervention were excluded. The participants' pain levels were recorded before and shortly after the intervention.Results: Women aged between 18 and 27 years (mean 22.8 ± 2.4 years) were evaluated. In addition to painful symptoms, all of them presented some other associated symptoms, the most common being diarrhea and fatigue (80%, each). The two-way ANOVA test of repeated measures considering group and evaluation factors revealed an effect only for the evaluation factor (p < 0.001) with no effect for the group/evaluation interaction (p = 0.09). Conclusion: TENS and cryotherapy are efficient resources for relieving pain symptoms in women with PD, with no superiority between the approaches.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Azagew AW, Kassie DG, Walle TA. Prevalence of primary dysmenorrhea, its intensity, impact and associated factors among female students' at Gondar town preparatory school, Northwest Ethiopia. BMC Womens Health. 2020;20(1):5. https://doi.org/10.1186/s12905-019-0873-4 PMid:31906945 PMCid:PMC6945628
Osayande AS, Mehulic S. Diagnosis and initial management of dysmenorrhea. Am Fam Physician. 2014;89(5):341-6
Kho KA, Shields JK. Diagnosis and management of primary dysmenorrhea. JAMA. 2020;323(3):268-9. https://doi.org/10.1001/jama.2019.16921 PMid:31855238
Daily JW, Zhang X, Kim DS, Park S. Efficacy of Ginger for alleviating the symptoms of primary dysmenorrhea: a systematic review and meta-analysis of randomized clinical trials. Pain Med. 2015;16(12):2243-55. https://doi.org/10.1111/pme.12853 PMid:26177393
Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762-78. https://doi.org/10.1093/humupd/dmv039 PMid:26346058
Al-Matouq S, Al-Mutairi H, Al-Mutairi O, Abdulaziz F, Al-Basri D, Al-Enzi M, et al. Dysmenorrhea among high-school students and its associated factors in Kuwait. BMC Pediatr. 2019;19(1):80. https://doi.org/10.1186/s12887-019-1442-6 PMid:30885151 PMCid:PMC6421654
Hu Z, Tang L, Chen L, Kaminga AC, Xu H. Prevalence and risk factors associated with primary dysmenorrhea among chinese female university students: a cross-sectional study. J Pediatr Adolesc Gynecol. 2020;33(1):15-22. https://doi.org/10.1016/j.jpag.2019.09.004 PMid:31539615
Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36:104-13. https://doi.org/10.1093/epirev/mxt009 PMid:24284871
Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428-41. https://doi.org/10.1097/01.AOG.0000230214.26638.0c PMid:16880317
Committee on Adolescent Health Care. ACOG Committee Opinion No. 760: Dysmenorrhea and endometriosis in the adolescent. Obstet Gynecol. 2018;132(6):e249-e58. https://doi.org/10.1097/AOG.0000000000002978
Alsaleem MA. Dysmenorrhea, associated symptoms, and management among students at King Khalid University, Saudi Arabia: an exploratory study. J Family Med Prim Care. 2018;7(4):769-74. https://doi.org/10.4103/jfmpc.jfmpc_113_18 PMid:30234051 PMCid:PMC6131986
Burnett M, Lemyre M. No. 345-Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2017;39(7):585-95. https://doi.org/10.1016/j.jogc.2016.12.023 PMid:28625286
Feng X, Wang X. Comparison of the efficacy and safety of non-steroidal anti-inflammatory drugs for patients with primary dysmenorrhea: a network meta-analysis. Mol Pain. 2018;14:1744806918770320. https://doi.org/10.1177/1744806918770320 PMid:29587566 PMCid:PMC5987898
De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, et al. Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev. 2015;13(2):512-20. PMID: 26841639
Igwea SE, Tabansi-Ochuogu CS, Abaraogu UO. TENS and heat therapy for pain relief and quality of life improvement in individuals with primary dysmenorrhea: a systematic review. Complement Ther Clin Pract. 2016;24:86-91. https://doi.org/10.1016/j.ctcp.2016.05.001 PMid:27502806
Pinho LEE, Monteiro AKS, Pimenta AG, Santos ASA. Terapia manual no tratamento da dismenorreia primária: revisão sistemática. Rev Pesq Fisioter. 2017;7(2):224-32. https://doi.org/10.17267/2238-2704rpf.v7i2.1327
Malanga GA, Yan N, Stark J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad Med. 2015;127(1):57-65. https://doi.org/10.1080/00325481.2015.992719 PMid:25526231
Yeh ML, Hung YL, Chen HH, Wang YJ. Auricular acupressure for pain relief in adolescents with dysmenorrhea: a placebo-controlled study. J Altern Complement Med. 2013;19(4):313-8. https://doi.org/10.1089/acm.2011.0665 PMid:23130943
Coutaux A. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine. 2017;84(6):657-61. https://doi.org/10.1016/j.jbspin.2017.02.005 PMid:28219657
Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database Syst Rev. 2015(6):CD006142. https://doi.org/10.1002/14651858.CD006142.pub3
Proctor ML, Smith CA, Farquhar CM, Stones RW. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev. 2002(1):CD002123. https://doi.org/10.1002/14651858.CD002123
Bouzigon R, Grappe F, Ravier G, Dugue B. Whole- and partial-body cryostimulation/cryotherapy: Current technologies and practical applications. J Therm Biol. 2016;61:67-81. https://doi.org/10.1016/j.jtherbio.2016.08.009 PMid:27712663
Aktas YY, Karabulut N. The use of cold therapy, music therapy and lidocaine spray for reducing pain and anxiety following chest tube removal. Complement Ther Clin Pract. 2019;34:179-84. https://doi.org/10.1016/j.ctcp.2018.12.001 PMid:30712725
Cha NH, Sok SR. Effects of auricular acupressure therapy on primary dysmenorrhea for female high school students in South Korea. J Nurs Scholarsh. 2016;48(5):508-16. https://doi.org/10.1111/jnu.12238 PMid:27541067
Ortiz MI, Cortes-Marquez SK, Romero-Quezada LC, Murguia-Canovas G, Jaramillo-Diaz AP. Effect of a physiotherapy program in women with primary dysmenorrhea. Eur J Obstet Gynecol Reprod Biol. 2015;194:24-9. https://doi.org/10.1016/j.ejogrb.2015.08.008 PMid:26319652
Balaban B, Tok F. Gait disturbances in patients with stroke. PM R: the journal of injury function and rehabilitation. 2014;6(7):635-42. https://doi.org/10.1016/j.pmrj.2013.12.017 PMid:24451335
Chen CX, Ofner S, Bakoyannis G, Kwekkeboom KL, Carpenter JS. Symptoms-based phenotypes among women with dysmenorrhea: a latent class analysis. West J Nurs Res. 2018;40(10):1452-68. https://doi.org/10.1177/0193945917731778 PMid:28914180 PMCid:PMC5832523
Chen L, Tang L, Guo S, Kaminga AC, Xu H. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019;9(9):e026813. https://doi.org/10.1136/bmjopen-2018-026813 PMid:31537555 PMCid:PMC6756436
Kamel DM, Tantawy SA, Abdelsamea GA. Experience of dysmenorrhea among a group of physical therapy students from Cairo University: an exploratory study. J Pain Res. 2017;10:1079-85. https://doi.org/10.2147/JPR.S132544 PMid:28533696 PMCid:PMC5431709
Yang M, Chen X, Bo L, Lao L, Chen J, Yu S, et al. Moxibustion for pain relief in patients with primary dysmenorrhea: A randomized controlled trial. PLoS One. 2017;12(2):e0170952. https://doi.org/10.1371/journal.pone.0170952 PMid:28170396 PMCid:PMC5295763
Bernstein MT, Graff LA, Avery L, Palatnick C, Parnerowski K, Targownik LE. Gastrointestinal symptoms before and during menses in healthy women. BMC Womens Health. 2014;14:14. https://doi.org/10.1186/1472-6874-14-14 PMid:24450290 PMCid:PMC3901893
Navvabi Rigi S, Kermansaravi F, Navidian A, Safabakhsh L, Safarzadeh A, Khazaian S, et al. Comparing the analgesic effect of heat patch containing iron chip and ibuprofen for primary dysmenorrhea: a randomized controlled trial. BMC Womens Health. 2012;12:25. https://doi.org/10.1186/1472-6874-12-25 PMid:22913409 PMCid:PMC3492023
Bai HY, Bai HY, Yang ZQ. Effect of transcutaneous electrical nerve stimulation therapy for the treatment of primary dysmenorrheal. Medicine (Baltimore). 2017;96(36):e7959. https://doi.org/10.1097/MD.0000000000007959 PMid:28885348 PMCid:PMC6392990
Tugay N, Akbayrak T, Demirturk F, Karakaya IC, Kocaacar O, Tugay U, et al. Effectiveness of transcutaneous electrical nerve stimulation and interferential current in primary dysmenorrhea. Pain Med. 2007;8(4):295-300. https://doi.org/10.1111/j.1526-4637.2007.00308.x PMid:17610451
Peng WW, Tang ZY, Zhang FR, Li H, Kong YZ, Iannetti GD, et al. Neurobiological mechanisms of TENS-induced analgesia. Neuroimage. 2019;195:396-408. https://doi.org/10.1016/j.neuroimage.2019.03.077 PMid:30946953 PMCid:PMC6547049
Raimundo AKS, Sousa LA, Silveira RF, Cerqueira MCD, Rodrigues J, Dini PD. Dosagem de serotonina sistêmica após aplicação da eletroestimulação nervosa transcutânea (TENS) [Internet]. Fisioter Mov. 2009 [cited 2020 Nov 17];22(3):365-74. Avaiable from: https://periodicos.pucpr.br/index.php/fisio/article/download/19459/18799
Lauretti GR, Oliveira R, Parada F, Mattos AL. The New portable transcutaneous electrical nerve stimulation device was efficacious in the control of primary dysmenorrhea cramp pain. Neuromodulation. 2015;18(6):522-6. https://doi.org/10.1111/ner.12269 PMid:25655828
Piana LE, Garvey KD, Burns H, Matzkin EG. The cold, hard facts of cryotherapy in orthopedics. Am J Orthop. 2018;47(9). https://doi.org/10.12788/ajo.2018.0075 PMid:30296319