Cardiovascular risk in primary care: comparison between Framingham Score and waist circumference
Main Article Content
Abstract
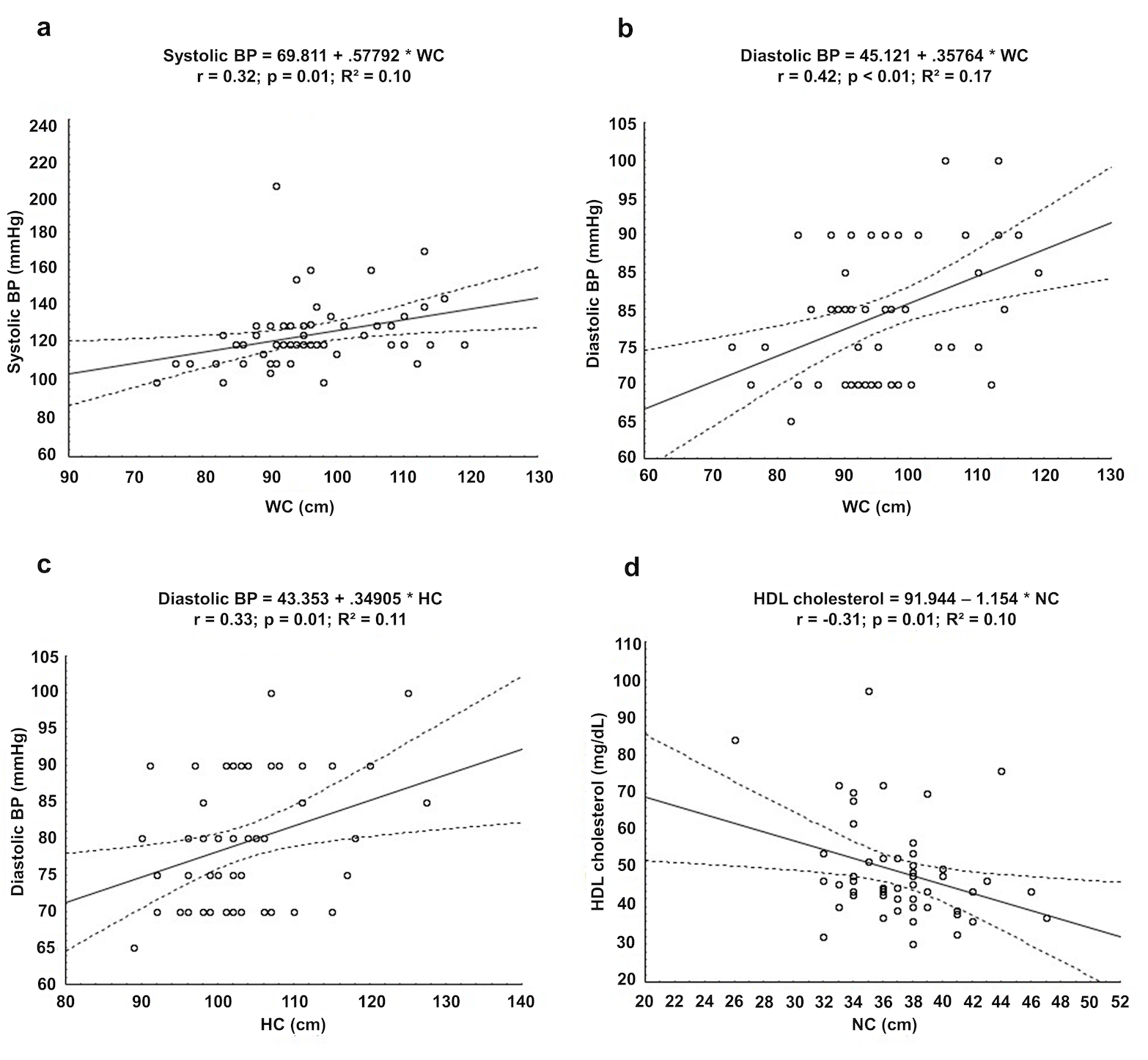
Objectives: To estimate and compare the cardiovascular risk using the Framingham risk score (FRS) and waist circumference (WC) in primary care individuals and, secondarily, determine the main factors associated with these scores. Methods: Cross-sectional study involving individuals of both sexes attended in a primary health unit and aging between 30 and 74 years. The cardiovascular risks (FRS and WC) were stratified as low, intermediate, and high. The weighted Kappa coefficient was used to assess agreements between scores. Results: Fifty-five individuals (52.8 ± 9.4 years, 70.9% women) were evaluated. Using the FRS, 40.0% of the sample presented a low risk, 45.5% intermediate risk, and 14.5% high risk of cardiovascular disease. Conversely, when analyzed using the WC score, the highest frequency (71%) was observed in the high-risk category. Also, no agreement (K= 0.36; p= 0.55) was found between scores. FRS was associated with hypertension (p<0.01), diabetes (p=0.01), and stress in women (p=0.01), while the WC score was associated with hypertension (p=0.02), obesity (p<0.01), and high-density lipoprotein cholesterol HDL-c (p=0.03). Conclusions: Primary care individuals presented intermediate cardiovascular risk in the FRS and high risk in the WC, with no agreement between scores. Hypertension, diabetes, stress, obesity, and HDL-c represented the factors that were most associated with these scores.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-646. https://doi.org/10.1161/CIR.0000000000000678
Gimbrone Jr MA, García-Cardeña G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res. 2016;118(4):620-36. https://doi.org/10.1161/CIRCRESAHA.115.306301 PMid:26892962 PMCid:PMC4762052
Reamy BV, Williams PM, Kuckel DP. Prevention of cardiovascular disease. Prim Care. 2018;45(1):25-44. https://doi.org/10.1016/j.pop.2017.11.003 PMid:29406943
Hajar R. Risk factors for coronary artery disease: Historical perspectives. Heart Views. 2017;18(3):109-14. https://doi.org/10.4103/HEARTVIEWS.HEARTVIEWS_106_17 PMid:29184622 PMCid:PMC5686931
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;73(24):3168-209. https://doi.org/10.1016/j.jacc.2018.11.002 PMid:30423391
Pitanga FJG, Matos SMA, Almeida MC, Barreto SM, Aquino EML. Leisure-time physical activity, but not commuting physical activity, is associated with cardiovascular risk among ELSA-Brasil participants. Arq Bras Cardiol. 2018;110(1):36-43. https://doi.org/10.5935/abc.20170178 PMid:29412240 PMCid:PMC5831300
Karmali KN, Persell SD, Perel P, Lloyd-Jones DM, Berendsen MA, Huffman MD. Risk scoring for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;3(3):CD006887. https://doi.org/10.1002/14651858.CD006887.pub4 PMid:28290160 PMCid:PMC6464686
Studzinski K, Tomasik T, Krzyszton J, Józwiak J, Windak A. Effect of using cardiovascular risk scoring in routine risk assessment in primary prevention of cardiovascular disease: an overview of systematic reviews. BMJ Open. 2019;19(11):1-16. https://doi.org/10.1186/s12872-018-0990-2 PMid:30626326 PMCid:PMC6327540
Damen JAAG, Hooft L, Shuit E, Debray TPA, Collins GS, Tzoulaki I, et al. Prediction models for cardiovascular disease risk in the general population: systematic review. BMJ. 2016;353:i2416. https://doi.org/10.1136/bmj.i2416 PMid:27184143 PMCid:PMC4868251
Jahangiry L, Farhangi MA, Rezaei F. Framingham risk score for estimation of 10-years of cardiovascular diseases risk in patients with metabolic syndrome. J Health Popul Nutr. 2017;36(1):36. https://doi.org/10.1186/s41043-017-0114-0 PMid:29132438 PMCid:PMC5682637
Rezende FAC, Rosado LEFPL, Ribeiro RCL, Vidigal FC, Vasques ACJ, Bonard IS, et al. Body mass index and waist circumference: association with cardiovascular risk factors. Arq Bras Cardiol. 2006;87(6):666-71. https://doi.org/10.1590/S0066-782X2006001900008 PMid:17262110
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477-500. https://doi.org/10.1161/CIRCRESAHA.120.316101 PMid:32437302
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-89. https://doi.org/10.1038/s41574-019-0310-7 PMid:32020062 PMCid:PMC7027970
Cibičková L', Langová K, Vaverková H, Lukeš J, Cibiček N, Karásek D. Superior role of waist circumference to body-mass index in the prediction of cardiometabolic risk in dyslipidemic patients. Physiol Res. 2019;68(6):931-8. https://doi.org/10.33549/physiolres.934176 PMid:31647298
Oliveira ACM, Ferreira RC, Santos AA. Cardiovascular risk assessment according to the Framingham Score and Abdominal Obesity in individuals seen by a clinical school of nutrition. Rev Assoc Med Bras. 2016;62(2):138-44. https://doi.org/10.1590/1806-9282.62.02.138 PMid:27167543
Abidov A, Chehab O. Cardiovascular risk assessment models: Have we found the perfect solution yet? J Nucl Cardiol. 2020;27(6):2375-85. https://doi.org/10.1007/s12350-019-01642-x PMid:30793251
Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. Diretrizes Brasileiras de Obesidade. [Internet]. 2016 [cited 2021 Nov 14]. Avaiable from: https://bit.ly/3oqBV6F
World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO Consultation on Obesity [Internet]. WHO: Geneva; 1997 [cited 2021 Nov 14]. Avaiable from: https://apps.who.int/iris/handle/10665/63854
D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743-53. https://doi.org/10.1161/CIRCULATIONAHA.107.699579 PMid:18212285
Grundy SM, Becker D, Clark LT, Cooper RS, Denke MA, Howard J, et al. Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143-421. https://doi.org/10.1161/circ.106.25.3143
Fleiss JL, Cohen J. The equivalence of weighted Kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613-9. https://doi.org/10.1177/001316447303300309
Lima Júnior MM, Silva GR, Jensem Filho SS, Granja F. Association between perceived lifetime risk of cardiovascular disease and calculated risk in a male population in Brazil. Vasc Health Risk Manag. 2016;12:279-86. https://doi.org/10.2147/VHRM.S107874 PMid:27382297 PMCid:PMC4922778
Motamed N, Perumal D, Zamani F, Ashrafi H, Haghjoo M, Saeedian FS, et al. Conicity index and waist-to-hip ratio are superior obesity indices in predicting 10-year cardiovascular risk among men and women. Clin Cardiol. 2015;38(9):527-34. https://doi.org/10.1002/clc.22437 PMid:26418518 PMCid:PMC6490781
Souza NC, Oliveira EP. Sagittal abdominal diameter shows better correlations with cardiovascular risk factors than waist circumference and BMI. J Diabetes Metab Disord. 2013;12:41. https://doi.org/10.1186/2251-6581-12-41 PMid:23856008 PMCid:PMC3733622
Bozorgmanesh M, Sardarinia M, Hajsheikholeslami F, Azizi F, Hadaegh F. CVD-predictive performances of "a body shape index" versus simple anthropometric measures: Tehran lipid and glucose study. Eur J Nutr. 2016;55(1):147-57. https://doi.org/10.1007/s00394-015-0833-1 PMid:25596850
Reis JP, Allen N, Gunderson EP, Lee JM, Lewis CE, Loria CM, et al. Excess body mass index- and waist circumference-years and incident cardiovascular disease: The CARDIA Study. Obesity (Silver Spring). 2015;23(4):879-85. https://doi.org/10.1002/oby.21023 PMid:25755157 PMCid:PMC4380633
Almeida RT, Matos SMA, Aquino EML. Individual and combined performance of indicators of overall and central obesity to estimate coronary risk in ELSA-Brasil participants. Arq Bras Cardiol. 2021;30:S0066-782X2021005011202. https://doi.org/10.36660/abc.20200360
Barroso TA, Marins LB, Alves R, Gonçalves ACS, Barroso SG, Rocha GS. Association of central obesity with the incidence of cardiovascular diseases and risk factors. Int J Cardiovasc Sci. 2017;30(5):416-24. https://doi.org/10.5935/2359-4802.20170073
Dimitriadis K, Tsioufis C, Mazaraki A, Liatakis I, Koutra E, Kordalis A, et al. Waist circumference compared with other obesity parameters as determinants of coronary artery disease in essential hypertension: a 6-year follow-up study. Hypertens Res. 2016;39(6):475-9. https://doi.org/10.1038/hr.2016.8 PMid:26865004
Sun H, Zheng M, Wu S, Chen M, Cai J, Yang X. Waist circumference and incidence of hypertension in chinese adults: observations from the Kailuan study. Herz. 2017;42(7):677-83. https://doi.org/10.1007/s00059-016-4501-x PMid:27928596
Tawfik HM. Waist height ratio and waist circumference in relation to hypertension, Framingham risk score in hospitalized elderly Egyptians. Egypt Heart J. 2018;70(3):213-6. https://doi.org/10.1016/j.ehj.2017.12.008 PMid:30190648 PMCid:PMC6123342
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring). 2011;19(5):1083-9. https://doi.org/10.1038/oby.2011.38 PMid:21372804 PMCid:PMC3275633
Lu N, Wang R, Ji M, Liu X, Qiang L, Ma C, et al. The value of hip circumference /height x ratio for identifying childhood hypertension. Sci Rep. 2018;8(1):3236. https://doi.org/10.1038/s41598-018-21676-4 PMid:29459689 PMCid:PMC5818505
Felix AS, Lehman A, Nolan TS, Sealy-Jefferson S, Breathett K, Hood DB, et al. Stress, resilience, and cardiovascular disease risk among black women. Circ Cardiovasc Qual Outcomes. 2019;12(4):e005284. https://doi.org/10.1161/CIRCOUTCOMES.118.005284 PMid:30909729 PMCid:PMC6508630
Magnavita N, Capitanelli I, Garbarino S, Pira E. Work-related stress as a cardiovascular risk factor in police officers: a systematic review of evidence. Int Arch Occup Environ Health. 2018;91(4):377-89. https://doi.org/10.1007/s00420-018-1290-y PMid:29344727
Dawber TR, Meadors GF, Moore Júnior FE. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health. 1951;41(3):279-86. https://doi.org/10.2105/AJPH.41.3.279 PMid:14819398 PMCid:PMC1525365
Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham Study. JAMA. 1987;257(16):2176-80. https://doi.org/10.1001/jama.257.16.2176 PMid:3560398
Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the honolulu heart program: a cohort study. Lancet. 2001;358(9279):351-5. https://doi.org/10.1016/S0140-6736(01)05553-2
Takata Y, Ansai T, Soh I, Awano S, Nakamichi I, Akifusa S, et al. Serum total cholesterol concentration and 10-year mortality in an 85-year-old population. Clin Interv Aging. 2014;9:293-300. https://doi.org/10.2147/CIA.S53754 PMid:24611005 PMCid:PMC3928456
Ascaso JF, Carmena R. Importance of dyslipidaemia in cardiovascular disease: a point of view. Clin Investig Arterioscler. 2015;27(6):301-8. https://doi.org/10.1016/j.arteri.2015.07.002 PMid:26363575
Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390(10107):2050-62. https://doi.org/10.1016/S0140-6736(17)32252-3
Nicholls SJ, Nelson AJ. HDL and cardiovascular disease. Pathology. 2019;51(2):142-7. https://doi.org/10.1016/j.pathol.2018.10.017 PMid:30612759
Woudberg NJ, Goedecke JH, Lecour S. Protection from cardiovascular disease due to increased high-density lipoprotein cholesterol in african black populations: myth or reality? Ethn Dis. 2016;26(4):553-60. https://doi.org/10.18865/ed.26.4.553 PMid:27773983 PMCid:PMC5072485