Etiology and pathophysiology of fibromyalgia
Main Article Content
Abstract
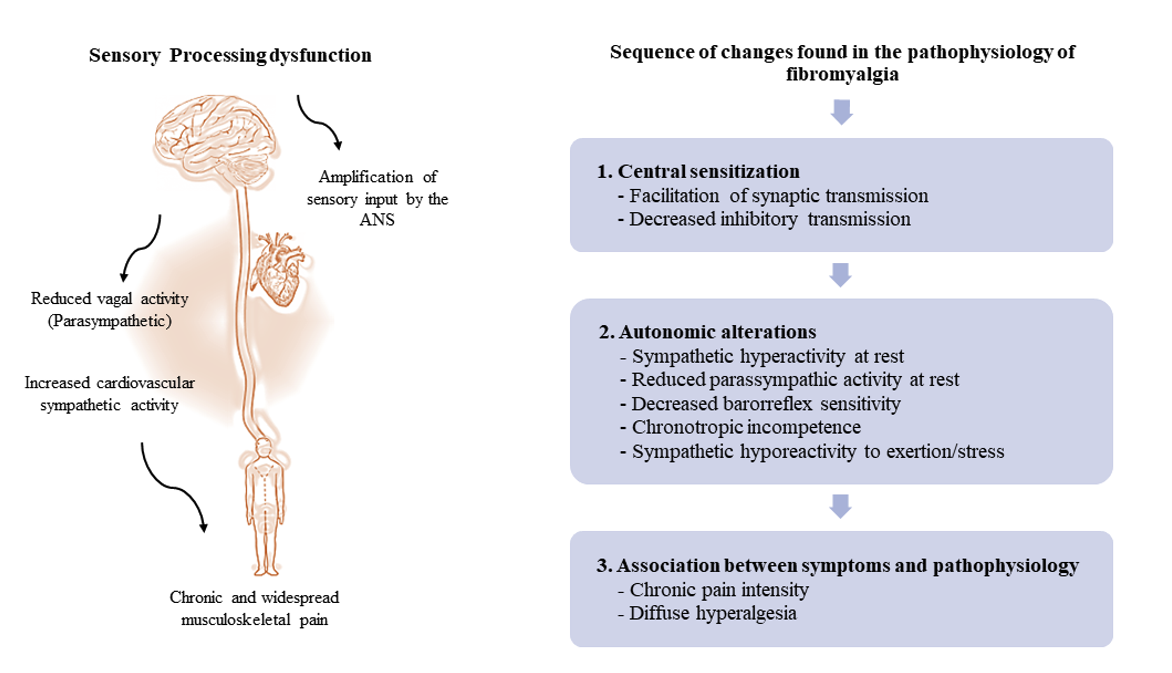
Fibromyalgia is a chronic condition of unknown etiology unrelated to specific laboratory markers for diagnosis because of poor etiopathogenesis. In general, the changes common to fibromyalgia are also seen in other chronic pain conditions, making the pathogenesis controversial among different pathological conditions. The unknown etiology makes the diagnosis difficult and consequently has repercussions on a not so effective treatment of patients with fibromyalgia. The restoration of systemic disorders provides a wide spectrum of therapeutic possibilities with the potential to guide professionals in establishing goals and evaluation methods. Therefore, this narrative review discusses the etiological and pathophysiological hypotheses involved in the development of fibromyalgia.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Cavalcante AB, Sauer JF, Chalot SD, Assumpção A, Lage L V, Akemi Matsutani L, et al. The Prevalence of Fibromyalgia: a Literature Review. Rev Bras Reum. 2006;46(1):40-8. https://doi.org/10.1590/S0482-50042006000100009
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003-7. https://doi.org/10.1097/j.pain.0000000000000160
Cabo-meseguer A, Cerdá-olmedo G, Trillo-mata L. Fibromialgia: prevalencia , perfiles epidemiológicos y costes económicos. 2017;149(10):441-8. https://doi.org/10.1016/j.medcli.2017.06.008
Souza JB, Perissinotti DMN. The prevalence of fibromyalgia in Brazil - a population-based study with secondary data of the study on chronic pain prevalence in Brazil. Brazilian J Pain. 2018;1(4):345-8. https://doi.org/10.5935/2595-0118.20180065
Maffei ME. Fibromyalgia: Recent advances in diagnosis, classification, pharmacotherapy and alternative remedies. Int J Mol Sci. 2020;21(21):7877. https://doi.org/10.3390/ijms21217877
Siracusa R, Paola RD, Cuzzocrea S, Impellizzeri D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int J Mol Sci. 2021;22(8):3891. https://doi.org/10.3390/ijms22083891
Briones-Vozmediano E, Vives-Cases C, Ronda-Pérez E, Gil-González D. Patients' and professionals' views on managing fibromyalgia. Pain Res Manag. 2013;18(1):19-24. https://doi.org/10.1155/2013/742510
Marques AP, Santo ASE, Berssaneti AA, Matsutani LA, Yuan SLK. A prevalência de fibromialgia: atualização da revisão de literatura. Rev Bras Reumatol. 2017;57(4):356-63. https://doi.org/10.1016/j.rbr.2016.10.004
Wolfe F, Walitt B, Perrot S, Rasker JJ, Häuser W. Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias. PLoS One. 2018;13(9):e0203755. https://doi.org/10.1371/journal.pone.0203755
Font Gayà T, Bordoy Ferrer C, Juan Mas A, Seoane-Mato D, Álvarez Reyes F, Delgado Sánchez M, et al; Working Group Proyecto EPISER2016. Prevalence of fibromyalgia and associated factors in Spain. Clin Exp Rheumatol. 2020;38 Suppl 123(1):47-52.
Heidari F, Afshari M, Moosazadeh M. Prevalence of fibromyalgia in general population and patients, a systematic review and meta-analysis. Rheumatol Int. 2017;37(9):1527-39. https://doi.org/10.1007/s00296-017-3725-2
Häuser W, Brähler E, Ablin J, Wolfe F. Modified 2016 American College of Rheumatology Fibromyalgia Criteria, the Analgesic, Anesthetic, and Addiction Clinical Trial Translations Innovations Opportunities and Networks-American Pain Society Pain Taxonomy, and the Prevalence of Fibromyalgia. Arthritis Care Res. 2021;73(5):617-25. https://doi.org/10.1002/acr.24202
Jones GT, Atzeni F, Beasley M, Macfarlane GJ, Group E, Building P. The prevalence of fibromyalgia in the general population - a comparison of the American College of Rheumatology 1990, 2010 and modified 2010 classification criteria. Arthritis Rheumatol. 2015;67(2):568-75. https://doi.org/10.1002/art.38905
Berger A, Sadosky A, Dukes EM, Edelsberg J, Zlateva G, Oster G. Patterns of healthcare utilization and cost in patients with newly diagnosed fibromyalgia. Am J Manag Care. 2010;16(5 Suppl):126-37.
Palacio A, Uribe CL, Li H, Hanna J, Deminski M, Alvir J, et al. Financial and clinical characteristics of fibromyalgia: a case-control comparison. Am J Manag Care. 2010;16(5 Suppl):118-25.
Berger A, Dukes E, Martin S, Edelsberg J, Oster G. Characteristics and healthcare costs of patients with fibromyalgia syndrome. Int J Clin Pract. 2007;61(9):1498-508. https://doi.org/10.1111/j.1742-1241.2007.01480.x
Walitt B, Katz RS, Bergman MJ, Wolfe F. Three-Quarters of Persons in the US Population Reporting a Clinical Diagnosis of Fibromyalgia Do Not Satisfy Fibromyalgia Criteria: The 2012 National Health Interview Survey. PLoS One. 2016;11(6):e0157235. https://doi.org/10.1371/journal.pone.0157235
Winkelmann A, Perrot S, Schaefer C, Ryan K, Chandran A, Sadosky A, Zlateva G. Impact of fibromyalgia severity on health economic costs: results from a European cross-sectional study. Appl Health Econ Health Policy. 2011;9(2):125-36. https://doi.org/10.2165/11535250-000000000-00000
Lacasse A, Bourgault P, Choinière M. Fibromyalgia-related costs and loss of productivity: a substantial societal burden. BMC Musculoskelet Disord. 2016;17:168. https://doi.org/10.1186/s12891-016-1027-6
Choy E, Perrot S, Leon T, Kaplan J, Petersel D, Ginovker A, Kramer E. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv Res. 2010;10:102. https://doi.org/10.1186/1472-6963-10-102
Hackshaw K V., Aykas DP, Sigurdson GT, Plans M, Madiai F, Yu L, et al. Metabolic fingerprinting for diagnosis of fibromyalgia and other rheumatologic disorders. J Biol Chem. 2019;294(7):2555-68. https://doi.org/10.1074/jbc.RA118.005816
Sluka KA, Clauw DJ. Neurobiology of fibromyalgia and chronic widespread pain Kathleen. Neuroscience. 2016;338:114-29. https://doi.org/10.1016/j.neuroscience.2016.06.006
SchreibeR KL, Loggia ML, Kim J, Cahalan CM, NapadoW V, Edwards RR. Painful After-Sensations in Fibromyalgia are Linked to Catastrophizing and Differences in Brain Response in the Medial Temporal Lobe. J Pains. 2017;18(7):855-67. https://doi.org/10.1016/j.jpain.2017.02.437
Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015;90(5):680-92. https://doi.org/10.1016/j.mayocp.2015.03.014
Albrecht DS, MacKie PJ, Kareken DA, Hutchins GD, Chumin EJ, Christian BT, Yoder KK. Differential dopamine function in fibromyalgia. Brain Imaging Behav. 2016;10(3):829-39. https://doi.org/10.1007/s11682-015-9459-4
Kuchinad A, Schweinhardt P, Seminowicz DA, Wood PB, Chizh BA, Bushnell MC. Accelerated brain gray matter loss in fibromyalgia patients: Premature aging of the brain? J Neurosci. 2007;27(15):4004-7. https://doi.org/10.1523/JNEUROSCI.0098-07.2007
Robinson ME, Craggs JG, Price DD, Perlstein WM, Staud R. Gray Matter Volumes of Pain Related Brain Areas are Decreased in Fibromyalgia Syndrome. J Pain. 2011;12(4):436-43. https://doi.org/10.1016/j.jpain.2010.10.003
Flodin P, Martinsen S, Löfgren M, Bileviciute-Ljungar I, Kosek E, Fransson P. Fibromyalgia is associated with decreased connectivity between pain- and sensorimotor brain areas. Brain Connect. 2014;4(8):587-94. https://doi.org/10.1089/brain.2014.0274
Jensen KB, Petzke F, Carville S, Fransson P, Marcus H, Williams SCR, et al. Anxiety and depressive symptoms in fibromyalgia are related to poor perception of health but not to pain sensitivity or cerebral processing of pain. Arthritis Rheum. 2010;62(11):3488-95. https://doi.org/10.1002/art.27649
Bäckryd E, Tanum L, Lind AL, Larsson A, Gordh T. Evidence of both systemic inflammation and neuroinflammation in fibromyalgia patients, as assessed by a multiplex protein panel applied to the cerebrospinal fluid and to plasma. J Pain Res. 2017;10:515-25. https://doi.org/10.2147/JPR.S128508
Kosek E, Altawil R, Kadetoff D, Finn A, Westman M, Le Maître E, et al. Evidence of different mediators of central inflammation in dysfunctional and inflammatory pain - Interleukin-8 in fibromyalgia and interleukin-1 β in rheumatoid arthritis. J Neuroimmunol. 2015;280:49-55. https://doi.org/10.1016/j.jneuroim.2015.02.002
Albrechta DS, Forsbergb A, Sandstrom A, Bergana C, Kadetoffc D, Protsenkoa E, et al. Brain glial activation in fibromyalgia - a multi-site positron emission tomography investigation. Brain Behav Immun. 2019;75:72-83. https://doi.org/10.1016/j.bbi.2018.09.018
Di Carlo M, Cesaroni P, Salaffi F. Neuropathic pain features suggestive of small fibre neuropathy in fibromyalgia syndrome: A clinical and ultrasonographic study on female patients. Clin Exp Rheumatol. 2021;39(130):102-7. https://doi.org/10.55563/clinexprheumatol/r0kho4
Kelley MA, Hackshaw K V. Intraepidermal nerve fiber density as measured by skin punch biopsy as a marker for small fiber neuropathy: Application in patients with fibromyalgia. Diagnostics. 2021;11(3):536. https://doi.org/10.3390/diagnostics11030536
Viceconti A, Geri T, De Luca S, Maselli F, Rossettini G, Sulli A, et al. Neuropathic pain and symptoms of potential small-fiber neuropathy in fibromyalgic patients: A national on-line survey. Jt Bone Spine. 2021;88(4):105153. https://doi.org/10.1016/j.jbspin.2021.105153
Grayston R, Czanner G, Elhadd K, Goebel A, Frank B, Üçeyler N, et al. A systematic review and meta-analysis of the prevalence of small fiber pathology in fibromyalgia: Implications for a new paradigm in fibromyalgia etiopathogenesis. Semin Arthritis Rheum. 2019;48(5):933-40. https://doi.org/10.1016/j.semarthrit.2018.08.003
Hulens M, Dankaerts W, Stalmans I, Somers A, Vansant G, Rasschaert R, et al. Fibromyalgia and unexplained widespread pain: The idiopathic cerebrospinal pressure dysregulation hypothesis. Med Hypotheses. 2018;110:150-4. https://doi.org/10.1016/j.mehy.2017.12.006
Hulens M, Bruyninckx F, Rasschaert R, Vansant G, De Mulder P, Stalmans I, et al. Electrodiagnostic abnormalities associated with fibromyalgia. J Pain Res. 2020;13:737-44. https://doi.org/10.2147/JPR.S234475
Hazra S, Venkataraman S, Handa G, Yadav SL, Wadhwa S, Singh U, et al. A cross-sectional study on central sensitization and autonomic changes in fibromyalgia. Front Neurosci. 2020;14:788. https://doi.org/10.3389/fnins.2020.00788
Harte SE, Harris RE, Clauw DJ. The neurobiology of central sensitization. J Appl Biobehav Res. 2018;23(2):e12137. https://doi.org/10.1111/jabr.12137
Fleming KC, Volcheck MM. Central Sensitization Syndrome and the Initial Evaluation of a Patient with Fibromyalgia: A Review. Rambam Maimonides Med J. 2015;6(2):e0020.
https://doi.org/10.5041/RMMJ.10204
Ashmawi HA, Freire GMG. Peripheral and central sensitization. Rev Dor. 2016;17(Suppl 1):31-4. https://doi.org/10.5935/1806-0013.20160044
Jay GW, Barkin RL. Fibromyalgia. Dis Mon. 2015;61:66-111. https://doi.org/10.1016/j.disamonth.2015.01.002
Vincent A, McAllister SJ, Singer W, Toussaint LL, Sletten DM, Whipple MO, et al. A Report of the Autonomic Symptom Profile in Patients with Fibromyalgia. J Clin Rheumatol. 2014;20(2):106-8. https://doi.org/10.1097/RHU.0b013e3182a225dd
Martinez-Lavin M. Fibromyalgia: When distress becomes (Un)sympathetic pain. Pain Res Treat. 2012;2012:981565. https://doi.org/10.1155/2012/981565
Waxenbaum JA, Reddy V, Varacallo M. Anatomy, Autonomic Nervous System. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. https://pubmed.ncbi.nlm.nih.gov/30969667/
Gibbons CH. Basics of autonomic nervous system function. Handb Clin Neurol. 2019;160:407-18. https://doi.org/10.1016/B978-0-444-64032-1.00027-8
Gordan R, Gwathmey JK, Xie LH. Autonomic and endocrine control of cardiovascular function. World J Cardiol. 2015;7(4):204. https://doi.org/10.4330/wjc.v7.i4.204
Goldberger JJ, Arora R, Buckley U, Shivkumar K. Autonomic Nervous System Dysfunction: J Am Coll Cardiol. 2019;73(10):1189-206. https://doi.org/10.1016/j.jacc.2018.12.064
Kang JH, Kim JK, Hong SH, Lee CH, Choi BY. Heart rate variability for quantification of autonomic dysfunction in fibromyalgia. Ann Rehabil Med. 2016;40(2):301-9. https://doi.org/10.5535/arm.2016.40.2.301
Schwab JO, Eichner G, Schmitt H, Weber S, Coch M, Waldecker B. The relative contribution of the sinus and AV node to heart rate variability. Heart. 2003;89(3):337-8. https://doi.org/10.1136/heart.89.3.337
Dong JG. The role of heart rate variability in sports physiology (Review). Exp Ther Med. 2016;11(5):1531-6. https://doi.org/10.3892/etm.2016.3104
Hayano J, Yuda E. Pitfalls of assessment of autonomic function by heart rate variability. J Physiol Anthropol. 2019;38(1):3. https://doi.org/10.1186/s40101-019-0193-2
Garavaglia L, Gulich D, Defeo MM, Mailland JT, Irurzun IM. The effect of age on the heart rate variability of healthy subjects. PLoS One. 2021;16(10):e0255894. https://doi.org/10.1371/journal.pone.0255894
da Cunha Ribeiro RP, Roschel H, Artioli GG, Dassouki T, Perandini LA, Calich AL, et al. Cardiac autonomic impairment and chronotropic incompetence in fibromyalgia. Arthritis Res Ther. 2011;13(6):R190. https://doi.org/10.1186/ar3519
Rost S, Crombez G, Sütterlin S, Vögele C, Veirman E, Van Ryckeghem DML. Altered regulation of negative affect in patients with fibromyalgia: A diary study. Eur J Pain (United Kingdom). 2021;25(3):714-24. https://doi.org/10.1002/ejp.1706
Meeus M, Goubert D, De Backer F, Struyf F, Hermans L, Coppieters I, et al. Heart rate variability in patients with fibromyalgia and patients with chronic fatigue syndrome: A systematic review. Semin Arthritis Rheum. 2013;43(2):279-87. https://doi.org/10.1016/j.semarthrit.2013.03.004
Figueroa A, Kingsley JD, Mcmillan V, Panton LB. Resistance exercise training improves heart rate variability in women with fibromyalgia. Clin Physiol Funct Imaging. 2008;28(1):49-54.
Paso GAR del, Coba P de la. Reduced activity, reactivity and functionality of the sympathetic nervous system in fibromyalgia: An electrodermal study. PLoS One. 2020;15(10):e0244830. https://doi.org/10.1371/journal.pone.0244830
Glasgow A, Stone TM, Kingsley JD. Resistance Exercise Training on Disease Impact, Pain Catastrophizing and Autonomic Modulation in Women with Fibromyalgia. Int J Exerc Sci. 2017;10(8):1184-1195. PMID: 29399247
Gavi MBRO, Vassalo DV, Amaral FT, Macedo DCF, Gava PL, Dantas EM, et al. Strengthening exercises improve symptoms and quality of life but do not change autonomic modulation in fibromyalgia: A randomized clinical trial. PLoS One. 2014;9(3):e90767. https://doi.org/10.1371/journal.pone.0090767
Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: Current perspectives. J Pain Res. 2017;10:2815-26. https://doi.org/10.2147/JPR.S134775
Koenig J, Thayer JF, Falvay D, Clamor A, Wagner J, Jarczok MN, et al. Pneumogastric (vagus) nerve activity indexed by heart rate variability in chronic pain patients compared to healthy controls: A systematic review and meta-analysis. Pain Physician. 2016;19(1):E55-78. https://doi.org/10.36076/ppj/2016.19.E55
Molero-Chamizo A, Nitsche MA, Bolz A, Barroso RTA, Bailén JRA, Palomeque JCG, et al. Non-Invasive Transcutaneous Vagus Nerve Stimulation for the Treatment of Fibromyalgia Symptoms: A Study Protocol. Brain Sci. 2022;12(1):95. https://doi.org/10.3390/brainsci12010095
Zamunér AR, Barbic F, Dipaola F, Bulgheroni M, Diana A, Atzeni F, et al. Relationship between sympathetic activity and pain intensity in fibromyalgia. Clin Exp Rheumatol. 2015;33:S53-7.
Tracy LM, Ioannou L, Baker KS, Gibson SJ, Georgiou-Karistianis N, Giummarra MJ. Meta-analytic evidence for decreased heart rate variability in chronic pain implicating parasympathetic nervous system dysregulation. Pain. 2016;157(1):7-29. https://doi.org/10.1097/j.pain.0000000000000360
Le Fur Bonnabesse A, Cabon M, L'Heveder G, Kermarrec A, Quinio B, Woda A, et al. Impact of a specific training programme on the neuromodulation of pain in female patient with fibromyalgia (DouFiSport): A 24-month, controlled, randomised, double-blind protocol. BMJ Open. 2019;9(1):e023742. https://doi.org/10.1136/bmjopen-2018-023742
Hughson RL, Shoemaker JK. Autonomic responses to exercise: Deconditioning/inactivity. Auton Neurosci Basic Clin. 2014;188:32-5. https://doi.org/10.1016/j.autneu.2014.10.012
Zaffalon Júnior JR, Viana AO, de Melo GEL, De Angelis K. The impact of sedentarism on heart rate variability (HRV) at rest and in response to mental stress in young women. Physiol Rep. 2018;6(18):13873. https://doi.org/10.14814/phy2.13873
Tebar WR, Ritti-Dias RM, Mota J, Farah BQ, Saraiva BTC, Damato TMM, et al. Relationship between domains of physical activity and cardiac autonomic modulation in adults: a cross-sectional study. Sci Rep. 2020;10(1):155-10. https://doi.org/10.1038/s41598-020-72663-7
Sabharwal R, Rasmussen L, Sluka KA, Chapleau MW. Exercise prevents development of autonomic dysregulation and hyperalgesia in a mouse model of chronic muscle pain. Pain. 2016;157(2):387-398. https://doi.org/10.1097/j.pain.0000000000000330