Impacts of the pandemic on children and adolescents with cancer: scoping review
Main Article Content
Abstract
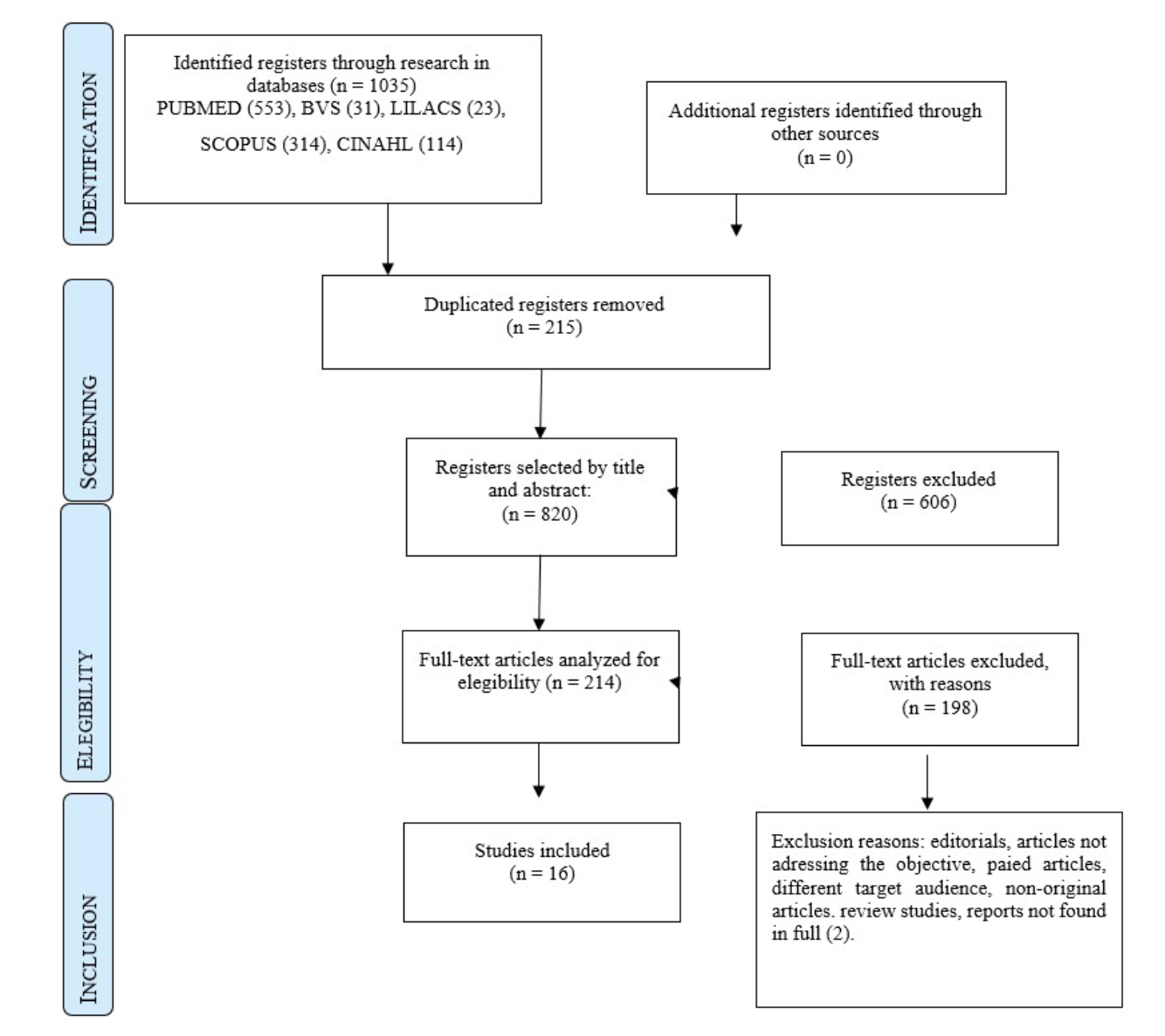
Objective: To identify the impacts of the COVID-19 pandemic on the health care of children and youth with oncological diseases. Method: Scoping review based on the Joanna Briggs Institute (JBI) methodological framework. To describe the research question, the population, concept, and context (PCC) strategy was used. The searches occurred in September 2022 in the BVS, Cinahl, Scopus, Lilacs, and PubMed databases, with the following descriptors: cancer; children; teenagers; pandemic; Covid; oncology; child; adolescent; and neoplasia. Rayyan software was used to select the studies, following the PRISMA recommendations. The content analysis method proposed by Bardin was used. Result: There were several impacts of the pandemic on care for children and adolescents’ oncology, related to daily life, the need to (re) organize health services, and, in this context, barriers were identified in maintaining treatment, postponing/reducing the offer of care, which impacted the reduction of specialized professionals and the supply of surgeries, and reduction of inputs and medicines. In the emotional sphere, the impacts were related to the intensification of feelings of fear and anxiety. Conclusion: In addition to the impacts caused by the pandemic, the need for awareness raising and support work for children and their families by primary care and specialized care teams became evident when they could not be assisted by other services, in addition to continued care at home.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Marques RC, Silveira AJT, Pimenta DN. A pandemia de Covid-19: intersecções e desafios para a história da saúde e do tempo presente. In: Reis TS, Souza CM, Oliveira MP, Lyra AA Jr, organizadores. Coleção História do Tempo Presente [Internet]. 3. ed. Roraima: Editora UFRR; 2020 [cited 2022 Oct 23]. v. 3, p. 225-249. Available from: https://www.ufrgs. br/redecovid19humanidades/index.php/br/colecao-historia-do-tempo-presente-volume-3
INCA: Instituto Nacional de Câncer. O que é câncer [Internet]. Brasília: INCA; 2022 [cited 2022 July 20]. Available from: https:// www.inca.gov.br/o-que-e-cancer
CCI: Childhood Câncer Internacional. Cura avançada, cuidado transformador [Internet]. 2022 [cited 2023 Feb 2]. Available from: https://www.childhoodcancerinternational.org/
SBP: Sociedade Brasileira de Pediatria. Câncer na criança e no adolescente [Internet]. Rio de Janeiro: SBP; 2022 [cited 2022 July 20]. Available from: https://www.sbp.com.br/especiais/ pediatria-para-familias/doencas/cancer-na-crianca-e-no-adolescente/
Santos PT Jr, Leite CQ, Teles IS, Barros IS No, Silva SM, Beduschi TF, et al. Aspectos epidemiológicos do Câncer Infantojuvenil em Porto Velho-RO no período de 2018 a 2020. Braz J Develop. 2022;8(2):12282-94. https://doi.org/10.34117/bjdv8n2-255. DOI: https://doi.org/10.34117/bjdv8n2-255
Peters MDJ, Godfrey C, McInerney P, Soares CB, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews [Internet]. Australia: The Joanna Briggs Institute; 2015 [cited 2022 Nov 28]. Available from: https://www.researchgate.net/publication/319713049_2017_ Guidance_for_the_Conduct_of_JBI_Scoping_Reviews
DocTranslator [Internet]. 2022 [cited 2022 Nov 28]. Available from: https://www.onlinedoctranslator.com/pt/translationform
Bardin L. Análise de conteúdo. 1. ed. São Paulo: Edições 70; 2011.
Sharma J, Mahajan A, Bakhshi S, Patil V, Verma N, Radhakrishnan V, et al. The impact of Covid‐19 pandemic on access to treatment for children with cancer in India and treating center practices. Cancer. 2021;128(3):579-86. http://doi.org/10.1002/cncr.33945. PMid:34618361. DOI: https://doi.org/10.1002/cncr.33945
Gopalakrishnan V, Veeraiah S, Chidambaram S, Sudhakar R, Radhakrishnan V. Caregiver’s perspective on psychosocial issues of paediatric cancer patients during Covid 19 pandemic lockdown. Psychooncology. 2022;31(6):1050-3. http://doi. org/10.1002/pon.5967. PMid:35578913. DOI: https://doi.org/10.1002/pon.5967
Atout M, Tarawneh FS, Al-Kharabsheh A. Challenges faced by mothers caring for children with leukaemia during COVID-19 pandemic: a qualitative study. J Ped Nurs. 2021;58:e74-80. http://doi.org/10.1016/j.pedn.2021.01.009. PMid:33526289. DOI: https://doi.org/10.1016/j.pedn.2021.01.009
Madhusoodhan PP, Pierro J, Musante J, Kothari P, Gampel B, Appel B, et al. Characterization of Covid‐19 disease in pediatric oncology patients: the New York‐New Jersey regional experience. Pediatr Blood Cancer. 2021;68(3):e28843. http:// doi.org/10.1002/pbc.28843. PMid:33338306. DOI: https://doi.org/10.1002/pbc.28843
Dvori M, Elitzur S, Barg A, Barzilai-Birenboim S, Gilad G, Amar S, et al. Delayed diagnosis and treatment of children with cancer during the Covid-19 pandemic. Int J Clin Oncol. 2021;26(8):1569-74. http://doi.org/10.1007/s10147-021-01971- 3. PMid:34145514. DOI: https://doi.org/10.1007/s10147-021-01971-3
Dotto C, Montanaro M, Spaggiari S, Cecinati V, Brescia L, Insogna S, et al. Early evidence of the interplay between separation anxiety symptoms and Covid-19-related worries in a group of children diagnosed with cancer and their mothers. Children (Basel). 2022;9(4):481. http://doi.org/10.3390/children9040481. PMid:35455525. DOI: https://doi.org/10.3390/children9040481
Graetz D, Agulnik A, Ranadive R, Vedaraju Y, Chen Y, Cantada G, et al. Global effect of the Covid-19 pandemic on paediatric cancer care: a cross-sectional study. Lancet Child Adolesc Health. 2021;5(5):332-40. http://doi.org/10.1016/S2352- 4642(21)00031-6. PMid:33675698. DOI: https://doi.org/10.1016/S2352-4642(21)00031-6
Sindhu II, Sarfraz S, Shaheen N, Khan A, Saeed H. Impact of Covid-19 pandemic on treatment of pediatric oncology patients: report from resource-limited setting. J Coll Physicians Surg Pak. 2021;31(11):1372-4. http://doi.org/10.29271/jcpsp.2021.11.1372. PMid:34689503. DOI: https://doi.org/10.29271/jcpsp.2021.11.1372
Saab R, Obeid A, Gachi F, Boudiaf H, Sargsyan L, Al-Saad K, et al. Impact of the coronavirus disease 2019 (Covid‐19) pandemic on pediatric oncology care in the Middle East, North Africa, and West Asia region: a report from the Pediatric Oncology East and Mediterranean (POEM) group. Cancer. 2020;126(18):4235-45. http://doi.org/10.1002/cncr.33075. PMid:32648950. DOI: https://doi.org/10.1002/cncr.33075
Erdmann F, Wellbrock M, Trubenbach C, Spix C, Schrappe M, Schütz D, et al. Impact of the Covid-19 pandemic on incidence, time of diagnosis and delivery of healthcare among paediatric oncology patients in germany in 2020: evidence from the german childhood cancer registry and a qualitative survey. The Lancet Regional Health-Europe. 2021;9:100188. http:// doi.org/10.1016/j.lanepe.2021.100188. PMid:34514453. DOI: https://doi.org/10.1016/j.lanepe.2021.100188
Global Health Research Group on Children’s Non-Communicable Diseases Collaborative. Impact of the Covid-19 pandemic on patients with paediatric cancer in low-income, middle-income and high-income countries: a multicentre, international, observational cohort study. BMJ Open. 2022;12(4):e054690. PMid:35410925. DOI: https://doi.org/10.1136/bmjopen-2021-054690
Wimberly CE, Towry L, Caudill C, Johnston EE, Walsh KM. Impacts of Covid‐19 on caregivers of childhood cancer survivors. Pediatr Blood Cancer. 2021;68(4):e28943. http://doi.org/10.1002/ pbc.28943. PMid: 33565259. DOI: https://doi.org/10.1002/pbc.28943
Davies J, O’Connor M, Halkett GKB, Kelada L, Gottardo NG. Parents’ experiences of childhood cancer during the COVID-19 pandemic: an Australian perspective. J Pediatr Psychol. 2022;47(2):148-57. http://doi.org/10.1093/jpepsy/jsab125. PMid:34865100. DOI: https://doi.org/10.1093/jpepsy/jsab125
Van Gorp M, Maurice-Stam H, Teunissen LC, Kilsdonk E, van Dijk J, Sulkers M, et al. Psychosocial function of dutch children with cancer and their caregivers during different phases of the Covid‐19 pandemic. Pediatr Blood Cancer. 2022;69(4):e29535. http://doi.org/10.1002/pbc.29535. PMid:35107873. DOI: https://doi.org/10.1002/pbc.29535
Alshahrani M, Elyamany G, Sedick Q, Ibrahim W, Mohamed A, Othman M, et al. The impact of Covid-19 pandemic in children with cancer: a report from Saudi Arabia. Health Serv Insights. 2020;13:1178632920984161. http://doi. org/10.1177/1178632920984161. PMid:33447044. DOI: https://doi.org/10.1177/1178632920984161
Mirlashari J, Ebrahimpour F, Salisu WJ. War on two fronts: experience of children with cancer and their family during Covid-19 pandemic in Iran. J Pediatr Nurs. 2021;57:25-31. http://doi.org/10.1016/j.pedn.2020.10.024. PMid:33212343. DOI: https://doi.org/10.1016/j.pedn.2020.10.024
Ribeiro CM, Correa FM, Migowski A. Efeitos de curto prazo da pandemia de Covid-19 na realização de procedimentos de rastreamento, investigação diagnóstica e tratamento do câncer no Brasil: estudo descritivo, 2019-2020. Epidemiol Serv Saude. 2022;31(1):e2021405. http://doi.org/10.1590/ s1679-49742022000100010. DOI: https://doi.org/10.1590/s1679-49742022000100010
Magalhães APFJ, Tomaz VS, Borges BMC, Pacífico AACP, Feitosa ESL, Vidal PA. A pandemia de COVID-19 e seu impacto na cirurgia. RevCienti HMJMA. 2022;3(1):28-33. https://doi. org/10.54257/2965-0585.v3.i1.3. DOI: https://doi.org/10.54257/2965-0585.v3.i1.3
Horta BL, Silveira MF, Barros AJD, Hartwig FP, Dias MS, Menezes AMB, et al. Covid-19 and outpatient care: a nationwide household survey. Cad Saude Publica. 2022;38(4):e00194121. http://doi. org/10.1590/0102-311x00194121. PMid:35442261. DOI: https://doi.org/10.1590/0102-311x00194121
Aquino EML, Silveira IH, Pescarini JM, Aquino R, Souza-Filho JA, Rocha AS, et al. Medidas de distanciamento social no controle da pandemia de Covid-19: potenciais impactos e desafios no Brasil. Cien Saude Colet. 2020;25(suppl 1):2423-46. http://doi. org/10.1590/1413-81232020256.1.10502020. PMid:32520287.
Quarello P, Ferrari A, Mascarin M, Milano GM, Tornesello A, Bertolotti M, et al. Diagnostic delay in adolescents with cancer during Covid-19 pandemic: a new price for our patients to pay. J Adolesc Young Adult Oncol. 2022;11(3):316-9. http:// doi.org/10.1089/jayao.2021.0057. PMid:34677087. DOI: https://doi.org/10.1089/jayao.2021.0057
Virnig BA, Nikpay SS. How will patients with cancer fare during Covid-19?: many unanswered questions. JAMA Oncol. 2021;7(2):195-6. http://doi.org/10.1001/jamaoncol.2020.6085. PMid:33270089. DOI: https://doi.org/10.1001/jamaoncol.2020.6085
Lee LYW, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, et al. Covid-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919-26. http://doi.org/10.1016/ S0140-6736(20)31173-9. PMid:32473682. DOI: https://doi.org/10.1016/S0140-6736(20)31173-9
Ganguly S, Bakhshi S. Continuing cancer-directed therapy in children with Covid-19 infection - adopting newer strategies? Indian J Pediatr. 2022;89(5):429-30. http://doi.org/10.1007/ s12098-022-04148-6. PMid:35212914. DOI: https://doi.org/10.1007/s12098-022-04148-6
Schwartz KM, Honstain C, Spruit JL, Harris M. Allogeneic hematopoietic stem cell transplant for acute lymphoblastic leukemia in a pediatric patient after Covid-19 infection complicated by MIS-C. J Pediatr Health Care. 2022;36(3):280-5. http://doi.org/10.1016/j.pedhc.2022.01.006. PMid:35256228. DOI: https://doi.org/10.1016/j.pedhc.2022.01.006
Vasquez L, Sampor C, Villanueva G, Maradiegue E, Garcia- Lombardi M, Gomez-García W, et al. Early impact of the Covid-19 pandemic on paediatric cancer care in Latin America. Lancet Oncol. 2020;21(6):753-5. http://doi.org/10.1016/S1470- 2045(20)30280-1. PMid:32437662. DOI: https://doi.org/10.1016/S1470-2045(20)30280-1
Sniderman ER, Graetz DE, Agulnik A, Ranadive R, Vedaraju Y, Chen Y, et al. Impact of the Covid‐19 pandemic on pediatric oncology providers globally: a mixed‐methods study. Cancer. 2022;128(7):1493-502. http://doi.org/10.1002/cncr.34090. PMid:35067925. DOI: https://doi.org/10.1002/cncr.34090
Kotecha RS. Challenges posed by Covid-19 to children with cancer. Lancet Oncol. 2020;21(5):e235. http://doi.org/10.1016/ S1470-2045(20)30205-9. PMid:32220660. DOI: https://doi.org/10.1016/S1470-2045(20)30205-9
Silva RS, Schmtiz CAA, Harzheim E, Molina-Bastos CG, Oliveira EB, Roman R, et al. O Papel da Telessaúde na Pandemia Covid-19: Uma Experiência Brasileira. Ciênc Saúde Coletiva. 2021 Jun;26(6):2149-57. https://doi.org/10.1590/1413- 81232021266.39662020. DOI: https://doi.org/10.1590/1413-81232021266.39662020
Silva LAGP, Orth BI, Alves das Mercês NN, Kalinke LP. Cuidado de crianças e adolescentes em tratamento oncológico na pandemia da Covid-19: experiência de familiares. Rev Enferm UERJ. 2023:e71271. http://doi.org/10.12957/reuerj.2023.71271. DOI: https://doi.org/10.12957/reuerj.2023.71271
Rymsza T, Lacerda JP, Trindade SHN. Effects of the Covid-19 pandemic on initial treatment of malignant neoplasms of the eye and appendices in children and adolescents. RSD. 2023;12(5):e0112541932. http://doi.org/10.33448/rsd-v12i5.41932. DOI: https://doi.org/10.33448/rsd-v12i5.41932