Mapping and projections of obesity in the Brazilian adult population assisted in Primary Health Care: impact of the COVID-19 pandemic
Main Article Content
Abstract
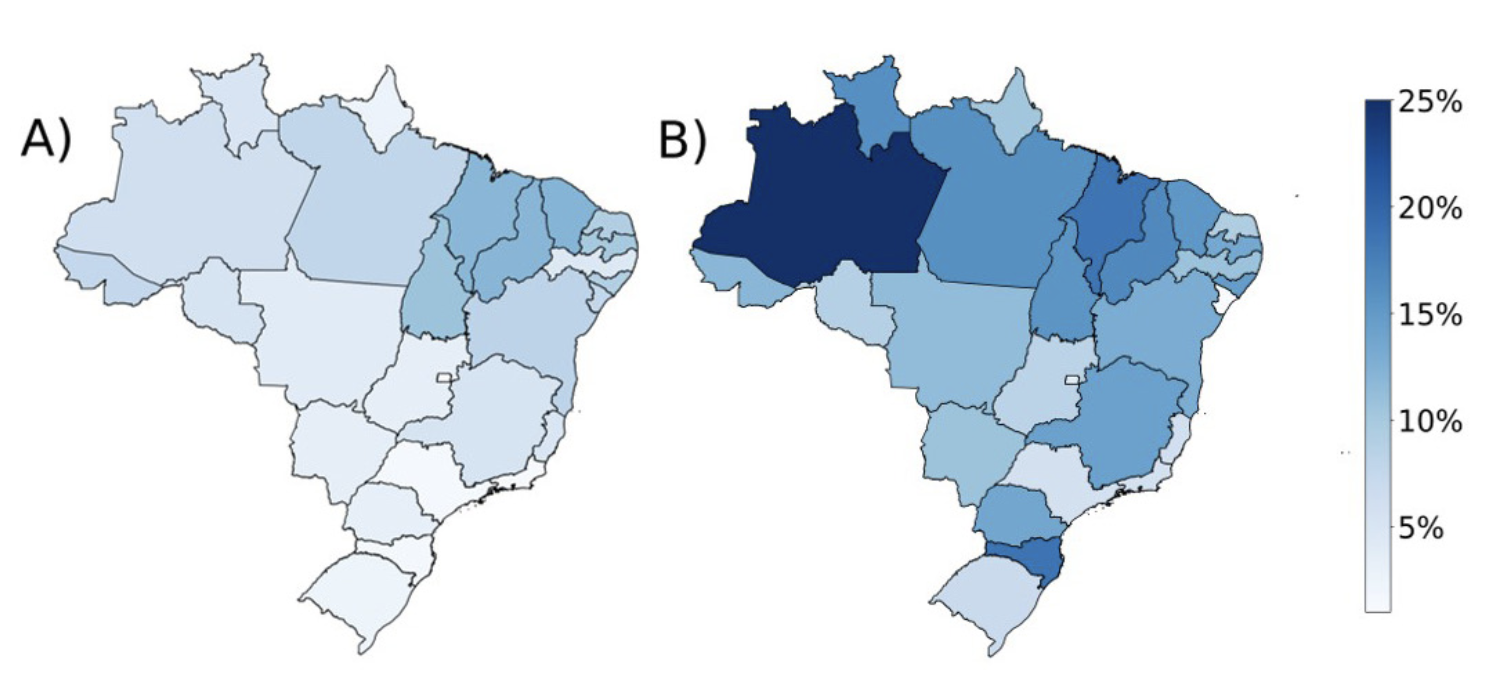
Objective: To map the temporal evolution of overweight and obesity in Brazilian adults and estimate the prevalence of obesity for 2025 and 2030, evaluating the potential impact of the COVID-19 pandemic. Method: Data were collected on the nutritional status of adults from 2008 to 2021 from the Food and Nutrition Surveillance System (SISVAN), from which we calculated the prevalence and average annual rates of the variation of overweight and obesity. The projection of obesity, using linear regression, was analyzed in three scenarios: PP: with data from the pre-pandemic period (2008- 2019); outlier: with adjustment of the data trend (2008-2021), including the pandemic period, considering a return of scenario PP for projections from 2022; P: adjustment of pandemic data (2019-2021) to estimate the projection. Result: In the period 2008– 2021, we observed an average annual rate of overweight increase of 0.48 %/year. The prevalence of obesity more than doubled during this period, from 14.5% in 2008 to 32.9% in 2021 (i.e., an increase of 1.42). In the outlier scenario, the prevalence projections for obesity are 38.8% and 45.5% for 2015 and 2030, respectively. In the PP scenario (without the pandemic), the expected prevalence for the same period would be approximately 36.8% and 43.4%, respectively. Conclusion: Obesity and overweight follow an increasing trend. The COVID-19 pandemic accelerated the increase in the prevalence of obesity in Brazil and impacted its projections for the coming years.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
WHO: World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: WHO; 2000. (WHO Technical Report Series).
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. http://doi.org/10.1186/1471-2458-9-88.PMid:19320986. DOI: https://doi.org/10.1186/1471-2458-9-88
Guo Y, Yue XJ, Li HH, Song ZX, Yan HQ, Zhang P, et al. Overweight and obesity in young adulthood and the risk of stroke: a meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(12):2995-3004. http://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.018.PMid:27618195. DOI: https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.018
Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. 2020;19(1):79. http://doi.org/10.1186/s12933-020-01052-1. DOI: https://doi.org/10.1186/s12933-020-01052-1
d’Errico M, Pavlova M, Spandonaro F. The economic burden of obesity in Italy: a cost-of-illness study. Eur J Health Econ. 2022;23(2):177-92. http://doi.org/10.1007/s10198-021-01358-1.PMid:34347176. DOI: https://doi.org/10.1007/s10198-021-01358-1
IBGE: Instituto Brasileiro de Geografia e Estatística. Coordenação de Trabalho e Rendimento. Pesquisa Nacional de Saúde: 2019: atenção primária à saúde e informações antropométricas. Rio de Janeiro: IBGE; 2020.
Global Burden of Disease Collaborative Network. Global Burden of Disease study 2019 (GBD 2019). Seattle: Institute for Health Metrics and Evaluation (IHME); 2021.
Nilson EAF, Santin Andrade RC, Brito DA, Oliveira ML. Costs attributable to obesity, hypertension, and diabetes in the Unified Health System, Brazil. Rev Panam Salud Publica. 2018;44:e32. http://doi.org/10.26633/RPSP.2020.32. DOI: https://doi.org/10.26633/RPSP.2020.32
Mrejen M, Cruz MV, Rosa L. O Sistema de Vigilância Alimentar e Nutricional (SISVAN) como ferramenta de monitoramento do estado nutricional de crianças e adolescentes no Brasil. Cad Saude Publica. 2023;39(1):e00169622. http://doi.org/10.1590/0102-311xpt169622.PMid:36856228. DOI: https://doi.org/10.1590/0102-311xpt169622
Boutari C, Mantzoros CSA. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217. PMid:35584732. DOI: https://doi.org/10.1016/j.metabol.2022.155217
Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. http://doi.org/10.3390/nu12061583.PMid:32481594.
Brasil. Ministério da Saúde. Sistema de Vigilância Alimentar e Nutricional – SISVAN. SISVAN-WEB [Internet]. Brasília: Ministério da Saúde; 2022 [cited 2022 Oct 20]. Available from: https://sisaps.saude.gov.br/sisvan/relatoriopublico/index
WHO: World Health Organization. WHO Expert Committee. Physical status: the use and interpretation of anthropometry. Geneva: WHO; 1995.
McKinney W. Data structures for statistical computing in Python. In: Proceedings of the 9th Python in Science Conference (SciPy 2010); 2010; local. Austin, Texas. Proceedings. SciPy; 2010. vol. 445. DOI: https://doi.org/10.25080/Majora-92bf1922-00a
Hunter JD. Matplotlib: a 2D graphics environvent. Comput Sci Eng. 2007;9(3):90-5. http://doi.org/10.1109/MCSE.2007.55. DOI: https://doi.org/10.1109/MCSE.2007.55
Waskom ML. Seaborn: statistical data visualization. J Open Source Softw. 2021;6(60):3021. http://doi.org/10.21105/joss.03021. DOI: https://doi.org/10.21105/joss.03021
IBGE: Instituto Brasileiro de Geografia e Estatística. Malha municipal. Rio de Janeiro: IBGE; 2021.
WHO: World Health Organization. Obesity and overweight [Internet]. 2021 [cited 2023 May 25]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight
WOF: World Obesity Federation. World obesity atlas 2023 [Internet]. London: WOF; 2023 [cited 2023 May 25]. Available from: www.johnclarksondesign.co.uk
WOF: World Obesity Federation. Obesity: missing the 2025 global targets. London: WOF; 2020. 242 p. [cited 2023 May 25]. Available from: https://data.worldobesity.org/publications/WOF-Missing-the-2025-Global-Targets-Report-FINAL-WEB.pdf
Costa CS, Steele EM, Leite MA, Rauber F, Levy RB, Monteiro CA. Body weight changes in the NutriNet Brasil cohort during the COVID-19 pandemic. Rev Saude Publica. 2021;55:1. http://doi.org/10.11606/s1518-8787.2021055003457. DOI: https://doi.org/10.11606/s1518-8787.2021055003457
Meller FO, Schäfer AA, Bianca LV, Viero VSF, Saes-Silva E, Quadra MR, et al. Home office is associated with weight gain during the Covid-19 pandemic: Brazilian population-based studies [Internet]. Ciência e Saúde Coletiva; 2023 [cited 2023 May 25]. Available from: http://cienciaesaudecoletiva.com.br/artigos/home-office-is-associated-with-weight-gain-during-the-covid19-pandemic-brazilian-populationbased-studies/18978?id=18978
Lee MN, Choi YS, Kim SD. The leading factors of obesity and severe obesity in Korean adults during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(19):12214. http://doi.org/10.3390/ijerph191912214.PMid:36231516. DOI: https://doi.org/10.3390/ijerph191912214
Restrepo BJ. Obesity prevalence among U.S. adults during the COVID-19 pandemic. Am J Prev Med. 2022;63(1):102-6. http://doi.org/10.1016/j.amepre.2022.01.012.PMid:35725124. DOI: https://doi.org/10.1016/j.amepre.2022.01.012
Bakaloudi DR, Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Chourdakis M. Impact of the first COVID-19 lockdown on body weight: a combined systematic review and a meta-analysis. Clin Nutr. 2022;41(12):3046-54. http://doi.org/10.1016/j.clnu.2021.04.015.PMid:34049749. DOI: https://doi.org/10.1016/j.clnu.2021.04.015
Park AH, Zhong S, Yang H, Jeong J, Lee C. Impact of COVID-19 on physical activity: a rapid review. J Glob Health. 2022;12:05003. http://doi.org/10.7189/jogh.12.05003.PMid:35493780. DOI: https://doi.org/10.7189/jogh.12.05003
Faria TMTR, Silva AG, Claro RM, Malta DC. Time trends and COVID-19 post-pandemic changes in physical activity and sedentary behavior prevalence among Brazilian adults between 2006 and 2021. Rev Bras Epidemiol. 2023;26(Suppl 1):e230011. http://doi.org/10.1590/1980-549720230011.supl.1. DOI: https://doi.org/10.1590/1980-549720230011.supl.1
Prado WL, Lofrano-Prado MC, Christofaro DGD, Santana CCA, Cucato GG, Jackson M, et al. The effects of COVID-19 stay-at-home orders on physical activity of people with obesity. Einstein. 2022;20:eAO6727. http://doi.org/10.31744/einstein_journal/2022AO6727.PMid:35476088. DOI: https://doi.org/10.31744/einstein_journal/2022AO6727
Clemmensen C, Petersen MB, Sørensen TIA. Will the COVID-19 pandemic worsen the obesity epidemic? Nat Rev Endocrinol. 2020;16(9):469-70. http://doi.org/10.1038/s41574-020-0387-z.PMid:32641837. DOI: https://doi.org/10.1038/s41574-020-0387-z
ACT Promoção da Saúde. Na pandemia, consumo de ultraprocessados quase dobra em faixa etária com maior risco [Internet]. 2020 [cited 2023 May 25]. Available from: https://actbr.org.br/post/na-pandemia-consumo-de-ultraprocessados-quase-dobra-em-faixa-etaria-com-maior-risco/18691/
IDEC: Instituto de Defesa do Consumidor. Pandemia: aumento de consumo de ultraprocessados pelo Brasil [Internet]. 2021 [cited 2023 May 25]. Available from: https://idec.org.br/noticia/pandemia-aumento-de-consumo-de-ultraprocessados-pelo-brasil
Menezes-Júnior LAA, Andrade ACS, Coletro HN, Mendonça RD, Menezes MC, Machado-Coelho GLL, et al. Food consumption according to the level of processing and sleep quality during the COVID-19 pandemic. Clin Nutr ESPEN. 2022;49:348-56. http://doi.org/10.1016/j.clnesp.2022.03.023.PMid:35623836. DOI: https://doi.org/10.1016/j.clnesp.2022.03.023
Malta DC, Szwarcwald CL, Barros MBA, Gomes CS, Machado IE, Souza PRB Jr, et al. A pandemia da COVID-19 e as mudanças no estilo de vida dos brasileiros adultos: um estudo transversal, 2020. Epidemiol Serv Saude. 2020;29(4):e2020407. http://doi.org/10.1590/s1679-49742020000400026.PMid:32997069. DOI: https://doi.org/10.1590/s1679-49742020000400026
Myers CA, Broyles ST. Fast food patronage and obesity prevalence during the COVID-19 pandemic: an alternative explanation. Obesity. 2020;28(10):1796-7. http://doi.org/10.1002/oby.22993.PMid:32741130. DOI: https://doi.org/10.1002/oby.22993
Oliveira LV, Rolim ACP, Silva GF, Araújo LC, Braga VAL, Coura AGL. Modificações dos hábitos alimentares relacionadas à pandemia do COVID-19: uma revisão de literatura. Braz J Health Rev. 2021;4(2):8464-77. http://doi.org/10.34119/bjhrv4n2-367. DOI: https://doi.org/10.34119/bjhrv4n2-367
Costa DVP, Lopes MS, Mendonça RD, Malta DC, Freitas PP, Lopes ACS. Food consumption differences in Brazilian urban and rural areas: the National Health Survey. Cien Saude Colet. 2021;26(Suppl 2):3805-13. PMid:34468674. DOI: https://doi.org/10.1590/1413-81232021269.2.26752019
WHO: World Health Organization. Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic [Internet]. Geneva: WHO; 2023 [cited 2023 May 25]. Available from: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
Lopes MS, Freitas PP, Carvalho MCR, Ferreira NL, Menezes MC, Lopes ACS. Is the management of obesity in primary health care appropriate in Brazil? Cad Saude Publica. 2021;37(Suppl 1):e00051620. http://doi.org/10.1590/0102-311x00051620.PMid:34932618. DOI: https://doi.org/10.1590/0102-311x00051620
Magalhães IF, Teixeira RA. Avaliação da implantação do SISVAN em municípios da jurisdição da superintendência regional de saúde de Diamantina/MG. Diamantina: Universidade Federal dos Vales do Jequitinhonha e Mucuri; 2019.