Animal models for inducing inflammatory bowel diseases: integrative review
Main Article Content
Abstract
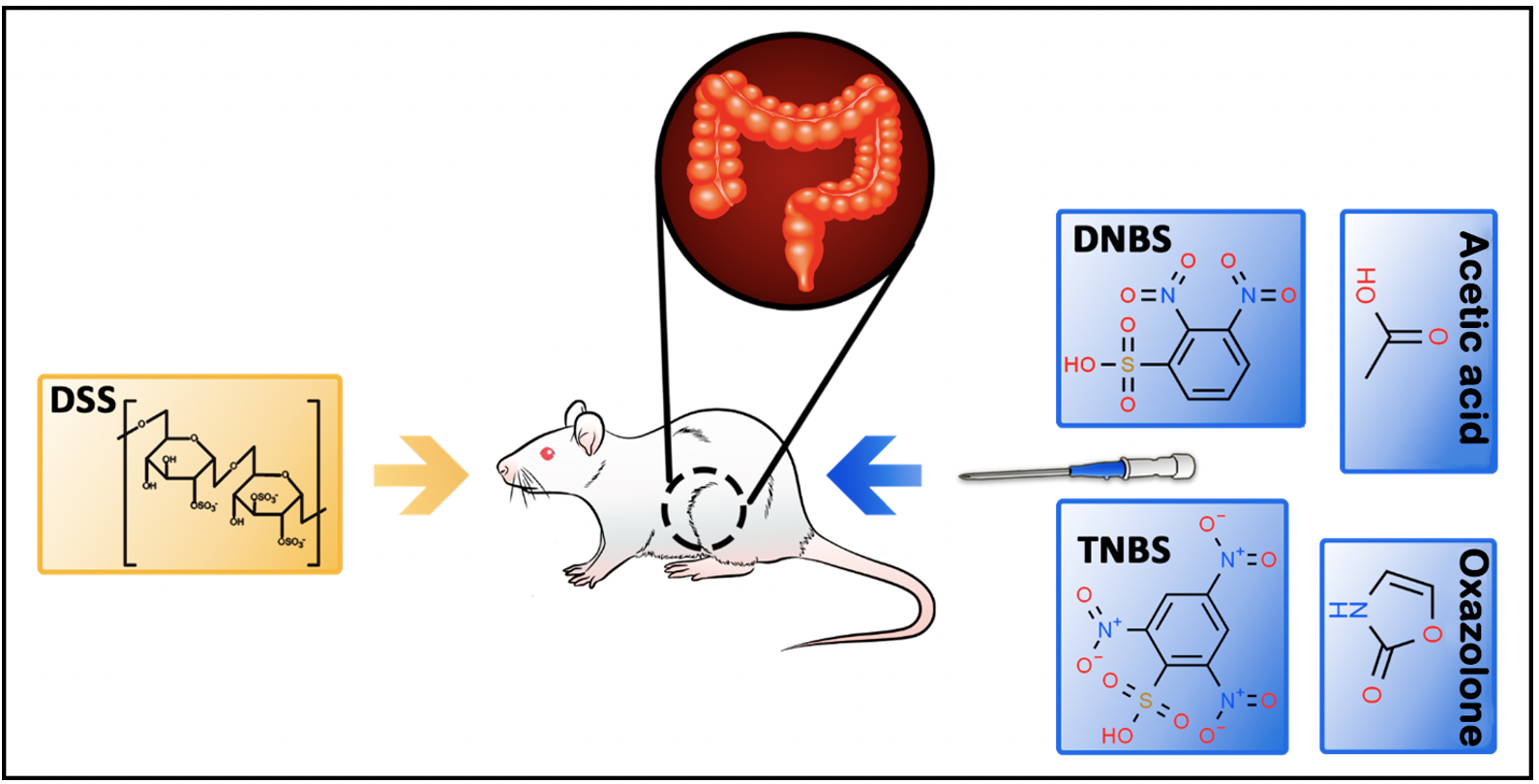
Objective: To identify and describe comparatively the chemical models of the induction of inflammatory bowel diseases (IBD) in rodents most used and that best mimic the pathogenesis in humans. Methods: Based on an integrative review in the MEDLINE and LILACS databases, it was investigated which experimental induction models were most cited in articles published from 2004 to 2020, with the descriptors "Colitis/CI", "Colitis model ulcerative" and "Intestinal inflammation model." All empirical articles that addressed one or more inflammation models in rats or mice were included. Results: 239 articles were identified; of these, only ten empirical articles were selected. The most used models were colitis induced by TNBS acid, DSS, and colitis induced by acetic acid (AA). Conclusion: It was possible to identify the most used models to promote the induction of intestinal inflammation in rats, and both models proved to be effective according to the limitations observed in the models described, suggesting the need for new works that use more well-defined protocols and that more fully represent the pathophysiological complexity of the disease.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Kleinubing-Júnior H, Pinho MSL, Ferreira LC, Bachtold GA, Merki A. Perfil dos pacientes ambulatoriais com doenças inflamatórias intestinais. Arq Bras Cir Dig. 2011;24(3):200-3. https://doi.org/10.1590/S0102-67202011000300004
Oliveira FM, Emerick APC, Soares EG. Aspectos epidemiológicos das doenças intestinais inflamatórias na macrorregião de saúde leste do Estado de Minas Gerais. Cienc Saúde Coletiva. 2010;15(Suppl 1):1031-7. https://doi.org/10.1590/S1413-81232010000700009 PMid:20640259
Sobrado CW, Sobrado LF. Management of acute severe ulcerative colitis: a clinical update. Arq Bras Cir Dig. 2016;29(3):201-5. https://doi.org/10.1590/0102-6720201600030017 PMid:27759787 PMCid:PMC5074675
Repka JCD, Caron PE, Belila RT, Antunes MW, Campos Filho JT, Bortolletto JT. Proposta de um novo modelo experimental de indução de doença inflamatória intestinal. Acta Cir Bras. 2004;19(5):548-54. https://doi.org/10.1590/S0102-86502004000500014
Hansen R, Thomson JM, El-Omar EM, Hold GL. The role of infection in the aetiology of inflammatory bowel disease. J Gastroenterol. 2010;45(3):266-76. https://doi.org/10.1007/s00535-009-0191-y PMid:20076977 PMCid:PMC7087869
Mota, ES, Kiss DR, Teixeira MG, Almeida MG, Sanfront FA, Habr-Gama A, et al. Manifestações extra-intestinais em doença de Crohn e retocolite ulcerativa: prevalência e correlação com o diagnóstico, extensão, atividade, tempo de evolução da doença. Rev Bras Colo-Proctol. 2007;27(4):349-63. https://doi.org/10.1590/S0101-98802007000400001
Gonçalves CCM, Hernandes L, Oliveira NLB, Natali MRM. Alternativas terapêuticas em modelos experimentais de doença inflamatória intestinal. Ciênc Cuid Saúde. 2008;7(1):107-11. https://doi.org/10.4025/cienccuidsaude.v7i0.6580
Russell B. História do pensamento ocidental. São Paulo: Ed. Publicações S/A; 2001.
Fagundes DJ, Taha MO. Modelo animal de doença: critérios de escolha e espécies de animais de uso corrente. Acta Cir Bras. 2004;19(1):59-65. https://doi.org/10.1590/S0102-86502004000100010
Jamwal S, Kumar P. Animal Models of Inflammatory Bowel Disease. In: Conn PM. Animal Models for the Study of Human Disease. Punjab: Elsevier, 2017. p. 467-477. https://doi.org/10.1016/B978-0-12-809468-6.00019-X
Brasil. Ministério da Saúde. Secretaria de Assistência à Saúde. Protocolo clínico e diretrizes terapêuticas para o tratamento de retocolite ulcerativa. Portaria SAS/MS n. 861 de 04 de novembro de 2002. Diário Oficial da União, Brasília (DF): Diário Oficial da União; 2002 [cited 2021 Mar 3]. Avaiable from: https://bit.ly/2PsHtjf
Rother ET. Revisão sistemática x revisão narrativa. Acta Paul Enferm. 2007;20(2):v-vi. https://doi.org/10.1590/S0103-21002007000200001
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-73. https://doi.org/10.7326/M18-0850 PMid:30178033
Babosa AS, Évora BR, Campos JS, Oliveira ES, Oliveira JN. Diminuição da susceptibilidade à clorexidina: revisão sistemática. J Infect Control [Internet]. 2019 [cited 2021 Mar 3];8(1):24-30. Avaiable from: https://jic-abih.com.br/index.php/jic/article/view/236
Câmara AB, de Oliveira Maia A, Oliveira JIN. O emprego da prototipagem rápida na engenharia tecidual. Biosaúde [Internet]. 2019 [cited 2021 Mar 3];20(1):19-37. Avaiable from: http://bit.ly/3sKpG5u
Campanelli SE, da Rocha JM, Oliveira JIN. Molecular and epigenetic mechanisms associated with extinction of fear memory: a systematic review. eNeurobiologia [Internet]. 2019 [cited 2021 Mar 3];10(24). Avaiable from: http://bit.ly/3e7z7b2
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. https://doi.org/10.2307/2529310 PMid:843571
Stillwell SB, Fineout-Overholt E, Melnyk MB, Williamson KM. Evidence-based practice, step by step: searching for the evidence. Am J Nurs. 2010;110(5);41-47. https://doi.org/10.1097/01.NAJ.0000372071.24134.7e PMid:20520115
Wirtz S, Kindermann A, Popp V, Gerlach K. Chemically induced mouse models of acute and chronic intestinal inflammation. Nat Protoc. 2017;12(7):1295-309. https://doi.org/10.1038/nprot.2017.044 PMid:28569761
Uhlig HH, Powrie F. Mouse models of intestinal inflammation as tools to understand the pathogenesis of inflammatory bowel disease. Eur J Immunol. 2009;39(8):2021-6. https://doi.org/10.1002/eji.200939602 PMid:19672896
Morampudi V, Bhinder G, Wu X, Dai C, Sham HP, Vallance BA, et al. DNBS/TNBS Colitis models: providing insights into inflammatory bowel disease and effects of dietary fat. J Vis Exp. 2014;(84):e51297. https://doi.org/10.3791/51297 PMid:24637969 PMCid:PMC4140598
Bertevello PL, Logullo FA, Nonogaki S, Campos FM, Chiferi V, Alves CC, et al. Immunohistochemical assessment of mucosal cytokine profile in acetic acid experimental colitis. Clinics. 2005;60(4):277-86. https://doi.org/10.1590/S1807-59322005000400004 PMid:16138233
Colares JR, Schemitt EG, Hartmann RM, Moura RM, Martins MIM, Fillmann HS, et al. Effect of lecithin on oxidative stress in an experimental model of rats colitis induced by acetic acid. J. Coloproctol. 2016;36(2):97-103. https://doi.org/10.1016/j.jcol.2016.03.002
Gheibi S, Hashemi SR, Karimipour M, Motlagh BM, Ghaleh HEG. Synergistic effects of hydro extract of jujube fruit in combination with Mesalazine (orally) and Asacol (intra-colonic) administration in ameliorating animal model of ulcerative colitis. J Coloproctol. 2018;38(4):275-82. https://doi.org/10.1016/j.jcol.2018.05.008
Karatepe O, Altiok M, Battal M, Kamali G, Kemik A, Aydin T, et al. The effect of progesterone in the prevention of the chemically induced experimental colitis in rats. Acta Cir Bras. 2012;27(1):23-9. https://doi.org/10.1590/S0102-86502012000100005 PMid:22159435
Marcelino MY, Fuoco NL, Quaglio AEV, Bittencourt RAC, Garms BC, Conceição THM, et al. Cell therapy in experimental model of inflammatory bowel disease. J Coloproctol. 2015;35(1):20-7. https://doi.org/10.1016/j.jcol.2014.06.004
Moura RM, Hartmann RM, Licks F, Schemitt EG, Colares JR, Soares MC, et al. Antioxidant effect of mesalazine in the experimental colitis model induced by acetic acid. J Coloproctol. 2016;36(3):139-48. https://doi.org/10.1016/j.jcol.2016.03.003
Oliveira LG, Cunha AL, Duarte AC, Castañon MCMN, Chebli JMF, Aguiar JAK. Positive correlation between disease activity index and matrix metalloproteinases activity in a rat model of colitis. Arq Gastroenterol. 2014;51(2):107-12. https://doi.org/10.1590/S0004-28032014000200007 PMid:25003261
Perera LMS, Batosta NY, Gálvez J, Duran R, Bulnes C. Rhizophora mangle L effect on experimental ulcerative colitis in rats. Rev Cuba Plantas Med [Internet]. 2009 [cited 2021 Mar 3];14(1):1-10. Avaiable from: http://scielo.sld.cu/pdf/pla/v14n1/pla07109.pdf
Zhong W, Xia Z, Hinrichs D, Rosenbaum JT, Wegmann KW, Meyrowitz J, et al. Hemin exerts multiple protective mechanisms and attenuates dextran sulfate sodium-induced colitis. J Pediatr Gastroenterol Nutr. 2010;50(2):132-9. https://doi.org/10.1097/MPG.0b013e3181c61591 PMid:20081544
Randhawa PK, Singh K, Singh N, Jaggi AS. A review on chemical-induced inflammatory bowel disease models in rodents. Korean J Physiol Pharmacol. 2014;18(4):279-88. https://doi.org/10.4196/kjpp.2014.18.4.279 PMid:25177159 PMCid:PMC4146629
Perše M, Cerar A. J Biomed Biotechnol.. Dextran sodium sulphate colitis mouse model: traps and tricks. 2012;2012:718617. https://doi.org/10.1155/2012/718617 PMid:22665990 PMCid:PMC3361365
Maxwell JR, Viney JL. Overview of mouse models of inflammatory bowel disease and their use in drug discovery. Curr Protoc Pharmacol. 2009; Chapter 5:Unit5.57. https://doi.org/10.1002/0471141755.ph0557s47 PMid:22294403
Kiesler P, Fuss IJ, Strober W. Experimental models of inflammatory bowel diseases. Cell Mol. Gastroenterol Hepatol. 2015;1(2):154-70. https://doi.org/10.1016/j.jcmgh.2015.01.006 PMid:26000334 PMCid:PMC4435576
Kolios G. Animal models of inflammatory bowel disease: how useful are they really? Curr Opin Gastroenterol. 2016;32(4):251-7. https://doi.org/10.1097/MOG.0000000000000287 PMid:27206158