Cross-cultural adaptation of the Subjective Index of Physical and Social Outcome (SIPSO) for application in Brazil
Main Article Content
Abstract
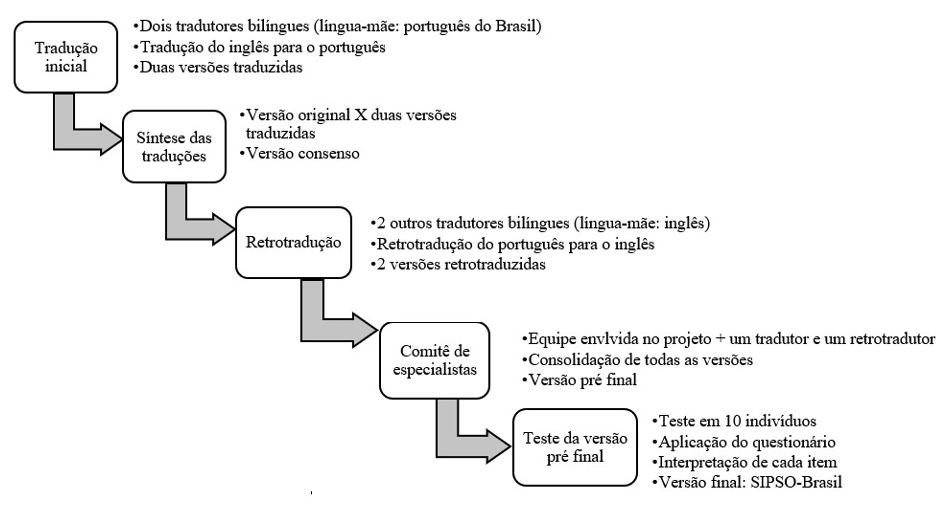
Objective: Participation restriction is a significant consequence for post-stroke individuals. In Brazil, there are no instruments available that comprehensively address participation in this population. Therefore, this study cross-culturally adapted the Subjective Index of Physical and Social Outcome (SIPSO) for use in Brazil. The SIPSO is a 10-item questionnaire covering participation questions considered significant for post-stroke individuals. Methods: The cross-cultural adaptation process involved the following steps: translation, back-translation, synthesis of translations, analysis by an expert committee and testing of the pre-final version. Results: Appropriate semantic equivalence was observed between the original and back-translated versions. During the expert meeting, the items were adapted to the grammatical rules of the Portuguese language. In the test of the pre-final version, one item of the instrument was reported as having difficulty in understanding, and an example was added to increase the possibility of understanding the item. Conclusion: SIPSO-Brasil presented a satisfactory degree of semantic, idiomatic, cultural, conceptual and operational equivalence. However, further studies must be conducted to continue the investigation of the validity of the adapted version of the instrument.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
2. BRASIL - MINISTÉRIO DA SAÚDE- Secretaria de Atenção à Saúde - Departamento de Ações Programáticas Estratégicas. Diretrizes de atenção à reabilitação da pessoa com acidente vascular cerebral [Internet]. BRASIL- MINISTÉRIO DA SAÚDE- Secretaria de Atenção à Saúde - Departamento de Ações Programáticas Estratégicas, editor. Brasília - DF; 2013. 72 p. Diusponível em: http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_atencao_reabilitacao_acidente_vascular_cerebral.pdf. Acesso em: 11/03/2021.
3. Alvarez-Sabín J, Quintana M, Masjuan J, Oliva-Moreno J, Mar J, Gonzalez-Rojas N, et al. Economic impact of patients admitted to stroke units in Spain. Eur J Health Econ. 2017;18:449-58. https://doi.org/10.1007/s10198-016-0799-9. PMID: 30871943.
4. Hewetson R, Cornwell P, Shum D. Social participation following right hemisphere stroke: influence of a cognitive-communication disorder. Aphasiology. 2018;32:164–82. https://doi.org/10.1080/02687038.2017.1315045. PMID: 28218007.
5. OMS. CIF: Classificação Internacional de Funcionalidade, Incapacidade e Saúde. [Internet]. EDUSP, editor. São Paulo; 2003. 216 p.
6. Wolf T, Brey J, Baum C, Connor L. Activity Participation Differences Between Younger and Older Individuals with Stroke. Brain Impair. 2012;13:16–23.
7. Desrosiers J, Bourbonnais D, Noreau L, Rochette A, Bravo G, Bourget A. Participation after stroke compared to normal aging. J Rehabil Med. 2005;37:353–7. https://doi.org/ 10.1080/16501970510037096. PMID: 16287666.
8. Ezeugwu VE, Manns PJ. Sleep Duration, Sedentary Behavior, Physical Activity, and Quality of Life after Inpatient Stroke Rehabilitation. J Stroke Cerebrovasc Dis. 2017;26:2004–12. https://doi.org/ 10.1016/j.jstrokecerebrovasdis.2017.06.009. PMID: 28669653.
9. Vincent-Onabajo GO, Hamzat TK, Owolabi MO. Consistent determinants of health-related quality of life in the first 12 months after stroke: a prospective study in Nigeria. Top Stroke Rehabil. 2015;22:127–33. https://doi.org/10.1179/1074935714Z.0000000033. PMID: 25936544.
10. Law M. Participation in the Occupations of Everyday Life. Am J Occup Ther. 2002;56:640–9. https://doi.org/10.5014/ajot.56.6.640. PMID: 12458856.
11. Obembe AO, Eng JJ. Rehabilitation Interventions for Improving Social Participation After Stroke: A Systematic Review and Meta-analysis. Neurorehabil Neural Repair. 2016;30(4):384–92. https://doi.org/ 10.1177/1545968315597072. PMID: 26223681.
12. Tse T, Douglas J, Lentin P, Carey L. Measuring participation after stroke: a review of frequently used tools. Arch Phys Med Rehabil. 2013;94(1):177–92. https://doi.org/10.1016/j.apmr.2012.09.002. PMID: 22982555.
13. Kossi O, Amanzonwe ER, Thonnard J-L, Batcho CS. Applicability of International Classification of Functioning, Disability and Health-based participation measures in stroke survivors in Africa: a systematic review. Int J Rehabil Res. 2020;43(1):3–11. https://doi.org/ 10.1097/MRR.0000000000000377. PMID: 3163358.
14. Carod-Artal FJ, Coral LF, Trizotto DS, Moreira CM. The stroke impact scale 3.0: evaluation of acceptability, reliability, and validity of the Brazilian version. Stroke. 2008;39:2477–84. https://doi.org/ 10.1161/STROKEAHA.107.513671. PMID: 18635846.
15. Monteiro M, Maso I, Sasaki AC, Barreto Neto N, Oliveira Filho J, Pinto EB. Validation of the Frenchay activity index on stroke victims. Arq Neuropsiquiatr. 2017;75:167–71. https://doi.org/ 10.1590/0004-282X20170014. PMID: 28355324.
16. Assumpção FSN, Faria-Fortini I, Basílio ML, Magalhães LC, Carvalho AC, Teixeira-Salmela LF. Adaptação transcultural do LIFE-H 3.1: um instrumento de avaliação da participação social . Cad Saúde Pública. 2016;32:S0102-311X2016000604001. https://doi.org/10.1590/0102-311X00061015. PMID: 27333131.
17. Veiga RFN, Morais AF, Nascimento SJN, Avelino PR, Costa HS, Menezes KKP de. Tradução, adaptação transcultural e confiabilidade da escala de utilidade clínica de Tyson e Connell . Fisioter Pesqui. 2020;27:78–84. https://doi.org/10.1590/1809-2950/19006227012020.
18. Trigg R, Wood VA, Hewer RL. Social reintegration after stroke: the first stages in the development of the Subjective Index of Physical and Social Outcome (SIPSO). Clin Rehabil. 1999;13:341–53. https://doi.org/ 10.1191/026921599676390259.
19. Trigg R, Wood VA. The Subjective Index of Physical and Social Outcome (SIPSO): a new measure for use with stroke patients. Clin Rehabil. 2000;14:288–99. https://doi.org/ 10.1191/026921500678119607. PMID: 10868724.
20. Lord S, McPherson KM, McNaughton HK, Rochester L, Weatherall M. How feasible is the attainment of community ambulation after stroke? A pilot randomized controlled trial to evaluate community-based physiotherapy in subacute stroke. Clin Rehabil. 2008;22:215–25. PMID: 18285431.
21. Harrington R, Taylor G, Hollinghurst S, Reed M, Kay H, Wood VA. A community-based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clin Rehabil. 2010;24(1):3–15. https://doi.org/ 10.1177/0269215509347437. PMID: 20026571.
22. Jones F, Mandy A, Partridge C. Changing self-efficacy in individuals following a first time stroke: preliminary study of a novel self-management intervention. Clin Rehabil. 2009;23:522–33. https://doi.org/10.1177/0269215508101749. PMID: 19403556.
23. Baseman S, Fisher K, Ward L, Bhattacharya A. The Relationship of Physical Function to Social Integration After Stroke. J Neurosci Nurs. 2010;42:237-44. https://doi.org/ 10.1097/jnn.0b013e3181ecafea. PMID: 20968219.
24. Trigg R, Wood VA. The validation of the Subjective Index of Physical and Social Outcome (SIPSO). Clin Rehabil. 2003;17:283–9. https://doi.org/10.1191/0269215503cr609oa. PMID: 12735535.
25. Kersten P, George S. The construct validity of the Subjective Index of Physical and Social Outcome (SIPSO). Clin Rehabil. 2004;18:931. https://doi.org/10.1191/0269215504cr835xx.
26. Teale EA, Young JB. A review of stroke outcome measures valid and reliable for administration by postal survey. Rev Clin Gerontol. 2010;20:338–53. https://doi.org/ 10.1017/S0959259810000213.
27. Kwong PW, Ng SS, Ng GY. An investigation of the psychometric properties of the Chinese (Cantonese) version of Subjective Index of Physical and Social Outcome (SIPSO). Clin Rehabil. 2017;31:1538–47. https://doi.org/ 10.1177/0269215517698736. PMID: 28343441.
28. Almeida C. Validação e Adaptação Cultural e Linguística do Subjective Index of Physical and Social Outcome (SIPSO).[Monografia]. Escola Superior de Tecnologia da Saúde de Coimbra; 2003.
29. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25:3186–91. https://doi.org/ 10.1097/00007632-200012150-00014.
30. Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8:94–104. https://doi.org/10.1111/j.1524-4733.2005.04054.x. PMID: 15804318.
31. Bertolucci PHF, Brucki SMD, Campacci SR, Juliano Y. O Mini-Exame do Estado Mental em uma população geral: impacto da escolaridade. Arq NeuroPsiquiatri. 1994;52:1-7. PMID: 8002795.
32. Coster W, Mancini M. Recomendações para a tradução e adaptação transcultural de instrumentos para a pesquisa e a prática em Terapia Ocupacional. Rev Ter Ocup da Univ São Paulo. 2015;26:50-7. http://dx.doi.org/10.11606/issn.2238-6149.v26i1p50-57.
33. Ribeiro LX, Braga CG, da Silva JV, Miranda RPR. Adaptação Transcultural da “Ways of Religious Coping Scale” (WORCS). Rev Cienc Saude 2015;5:18-4. https://doi.org/10.21876/rcsfmit.v5i1.312.
34. Faria-Fortini I, Basílio M, Assumpção F, Teixeira-Salmela L. Adaptação transcultural e reprodutibilidade do Measure of the Quality of the Enviroment em indivíduos com hemiparesia. Rev Ter Ocup Univ São Paulo. 2016;27:42-51. http://dx.doi.org/10.11606/issn.2238-6149.v27i1p42-51.
35. Basílio ML, Faria-Fortini I, Assumpção FSN, Carvalho AC, Teixeira-Salmela LF. Adaptação transcultural do Questionário ABILHAND específico para indivíduos pós-acidente vascular encefálico. Rev Ter Ocup Univ São Paulo. 2017;28:19-26. http://dx.doi.org/10.11606/issn.2238-6149.v28i1p19-26.
36. Marquito AB, Pinheiro HS, Paula RB. Adaptação transcultural do instrumento PAIR: Pharmacotherapy Assessment in Chronic Renal Disease para aplicação no Brasil . Ciênc Saúde Coletiva. 2020;25: 4021–32. https://doi.org/10.1590/1413-812320202510.35522018.
37. Salter K, Hellings C, Foley N, Teasell R. The experience of living with stroke: a qualitative meta-synthesis. J Rehabil Med. 2008;40:595–602. https://doi.org/10.2340/16501977-0238. PMID: 19020691.
38. Dijkers MP. Issues in the conceptualization and measurement of participation: an overview. Arch Phys Med Rehabil. 2010;91:S5-16. https://doi.org/ 10.1016/j.apmr.2009.10.036.
39. Lima A, Jr RC. Indicador de Alfabetismo Funcional (INAF) 2018 - Resultados preliminares. São Paulo; 2018. Disponível em: https://drive.google.com/file/d/1ez-6jrlrRRUm9JJ3MkwxEUffltjCTEI6/view. Acesso em: 11/03/2021.