Impacts of aerobic exercise on children with asthma diagnosis: integrative review
Main Article Content
Abstract
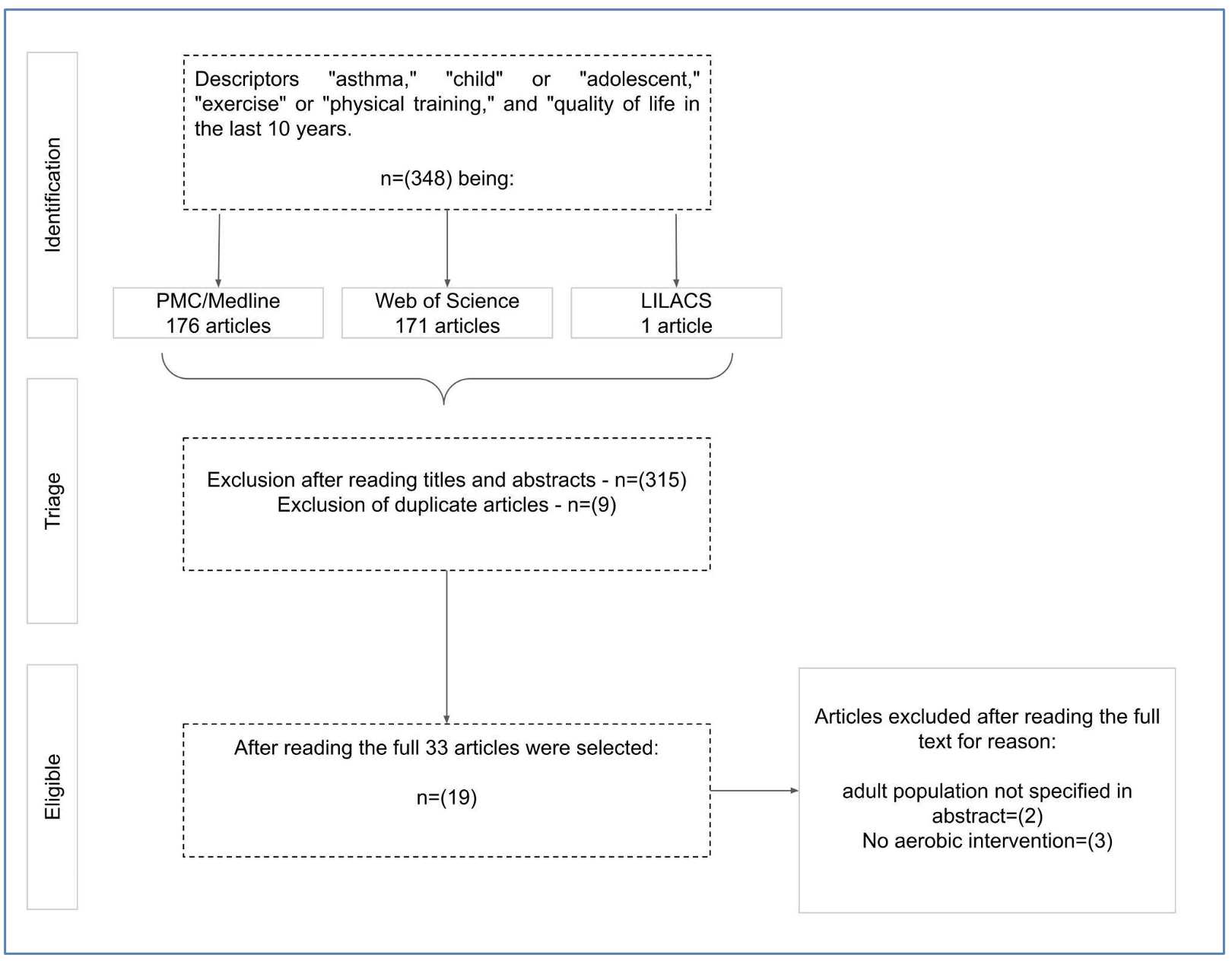
Objective: To identify the impacts of aerobic exercise on the health of children with asthma, seeking to know protocols of rehabilitation programs and their impacts. Methods: Clinical trials published from 2010 to 2020 were selected, filtered by the descriptors: 'asthma', 'exercise' or 'physical training', 'children' OR 'adolescents' AND 'quality of life'. Results: Nineteen articles were included; the duration of the programs ranged from 4 to 24 weeks, 2 to 6 times/week, with the sessions varying from 30 min to 1h10min and intensity from 40% to 100% of the Maximum Heart Rate. The studies evaluated strength, lung capacity and function, inflammatory mediators, quality of life, and asthma control. Aerobic interventions made it possible to improve cardiorespiratory capacity, intracellular action of antioxidants, quality of life, and disease control. Significant results were found in protocols with playful exercises performed for 60 minutes, three times a week, and at least 12 weeks. Conclusion: The ease of reproducing the protocols can provide greater coverage of care and rehabilitation, which in the long term can help to reduce the hospitalization rate, cost, and hospital demand for severe exacerbations.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes da Sociedade Brasileira de Pneumologia e Tisiologia para o manejo da asma. J Bras Pneumol, 2012;38(supl. 1): s1-46. DOI: https://doi.org/10.1590/S1806-37132012000300002
Forum of International Respiratory Societies. The Global Impact of Respiratory Disease – Second Edition. Sheffield, European Respiratory Society, 2017 [ cited 2022 Feb 24]. Avaiable from: https://www.who.int/gard/publications/The_Global_Impact_of_Respiratory_Disease_ES.pdf
Solé D, Camelo-Nunes IC, Wandalsen GF, Mallozi MC. A asma na criança e no adolescente brasileiro: contribuição do International Study of Asthma and Allergies in Childhood (ISAAC). Rev Paul Pediatr. 2014;32(1):114-25. https://doi.org/10.1590/S0103-05822014000100018 DOI: https://doi.org/10.1590/S0103-05822014000100018
Abdelbasset WK, Alsubaie SF, Tantawy SA, Abo Elyazed TI, Kamel DM. Evaluating pulmonary function, aerobic capacity, and pediatric quality of life following a 10-week aerobic exercise training in school-aged asthmatics: a randomized controlled trial. Patient Prefer Adherence. 2018;12:1015-23. https://doi.org/10.2147/PPA.S159622 DOI: https://doi.org/10.2147/PPA.S159622
Reimberg MM, Castro RAS, Selman JPR, Meneses AS, Politti F, Mallozi MC, et al. Patients with asthma have reduced functional capacity and sedentary behavior. J Pediatr (Rio J). 2020;96(1):53-9. https://doi.org/10.1016/j.jpedp.2018.11.004 DOI: https://doi.org/10.1016/j.jped.2018.07.011
Wicher IB, Ribeiro MAGO, Marmo DB, Santos CIS, Toro AADC, Mendes RT, et al. Effects of swimming on spirometric parameters and bronchial hyperresponsiveness in children and adolescents with moderate persistent atopic asthma. J Pediatr (Rio J). 2010;86(5):384-90. https://doi.org/10.2223/JPED.2022 DOI: https://doi.org/10.2223/JPED.2022
Onur E, Kabaroğlu C, Günay Ö, Var A, Yilmaz Ö, Dündar P, et al. The beneficial effects of physical exercise on antioxidant status in asthmatic children. Allergol Immunopathol (Madr), 2011;39(2):90-5. https://doi.org/10.1016/j.aller.2010.04.006 DOI: https://doi.org/10.1016/j.aller.2010.04.006
Gunay O, Onur E, Yilmaz O, Dundar PE, Tikiz C, Var A, at al. Effects of physical exercise on lung injury and oxidant stress in children with asthma. Allergol Immunopathol (Madr), 2012;40(1):20-4. https://doi.org/10.1016/j.aller.2010.10.006 DOI: https://doi.org/10.1016/j.aller.2010.10.006
Andrade LB, Britto MCA, Lucena-Silva N, Gomes RG, Figueroa JN. The efficacy of aerobic training in improving the inflammatory component of asthmatic children. Randomized trial. Respir Med. 2014;108(10):1438-45. https://doi.org/10.1016/j.rmed.2014.07.009 DOI: https://doi.org/10.1016/j.rmed.2014.07.009
Latorre-Román PA, Navarro-Martínez AV, García-Pinillos F. The effectiveness of an indoor intermittent training program for improving lung function, physical capacity, body composition and quality of life in children with asthma. J Asthma. 2014;51(5):544-51. https://doi.org/10.3109/02770903.2014.888573 DOI: https://doi.org/10.3109/02770903.2014.888573
Gomes ELFD, Carvalho CRF, Peixoto-Souza FS, Teixeira-Carvalho EF, Mendonça JFB, Stirbulov R, et al. Active video game exercise training improves the clinical control of asthma in children: randomized controlled trial. Plos One. 2015;10(8):0135433. https://doi.org/10.1371/journal.pone.0135433 DOI: https://doi.org/10.1371/journal.pone.0135433
Latorre-Román PA, Martínez AVN, García-Pinillos F. Efeito de um programa de atividade física no gozo do esporte, participação na atividade física, autoconceito físico e qualidade de vida em crianças asmáticas. Motriz. 2015;21(4):386-92. https://doi.org/10.1590/S1980-65742015000400007 DOI: https://doi.org/10.1590/S1980-65742015000400007
Westergren T, Fegran L, Nilsen T, Haraldstad K, Kittang OB, Berntsen S. Active play exercise intervention in children with asthma: a pilot study. BMJ Open. 2016;6(1):e009721. https://doi.org/10.1136/bmjopen-2015-009721 DOI: https://doi.org/10.1136/bmjopen-2015-009721
Lin H, Lin H, Yu H, Wang L, Lee J, Lin Y, et al. Tai-Chi-Chuan exercise improves pulmonary function and decreases exhaled nitric oxide level in both asthmatic and nonasthmatic children and improves quality of life in children with asthma. Evid Based Complement Alternat Med. 2017;2017:6287642. https://doi.org/10.1155/2017/6287642 DOI: https://doi.org/10.1155/2017/6287642
Willeboordse M, Kant KDG, Tan FES, Mulkens S, Schellings J, Crijns Y, et al. A multifactorial weight reduction programme for children with overweight and asthma: a randomized controlled trial. Plos One, 2016;11(6):e0157158. https://doi.org/10.1371/journal.pone.0157158 DOI: https://doi.org/10.1371/journal.pone.0157158
Kováčiková Z, Neumannova K, Rydlova J, Bizovská L, Janura M. The effect of balance training intervention on postural stability in children with asthma. J Asthma, 2017;55(5):502-10. https://doi.org/10.1080/02770903.2017.1342257 DOI: https://doi.org/10.1080/02770903.2017.1342257
Doğruel D, Altintaş DU, Yilmaz M. Astımlı çocuklarda fiziksel egzersizin klinik ve fonksiyonel parametrelere etkisi [Turkish]. Cukurova Med J. 2018;43(2):457-62. https://doi.org/10.17826/cumj.366166 DOI: https://doi.org/10.17826/cumj.366166
Lu KD, Cooper DM, Haddad F, Radam-Aizik S. Four months of a school-based exercise program improved aerobic fitness and clinical outcomes in a low-ses population of normal weight and overweight/obese children with asthma. Front Pediatr. 2018;6:380. https://doi.org/10.3389/fped.2018.00380 DOI: https://doi.org/10.3389/fped.2018.00380
Khodashenas E, Bakhtiari E, Sohrabi M, Mozayani A, Arabi M, Haghighi VV, et al. The effect of a selective exercise program on motor competence and pulmonary function of asthmatic children: a randomized clinical trial. International Int J Pediatr. 2019;7(7):9711-17. https://doi.org/10.22038/ijp.2019.37253.3243
Liao P, Lin H, Chiang B, Lee J, Yu H, Lin Y, et al. Tai Chi Chuan Exercise improves lung function and asthma control through immune regulation in childhood asthma. Evid Based Complement Alternat Med. 2019;2019:9146827. https://doi.org/10.1155/2019/9146827 DOI: https://doi.org/10.1155/2019/9146827
Mcnarry MA, Lewis MJ, Wade N, Davies GA, Winn C, Eddolls WTB,et al. Effect of asthma and six-months high-intensity interval training on heart rate variability during exercise in adolescents. Med Sci Sports Exerc. 2019;37(19):2228-35. https://doi.org/10.1080/02640414.2019.1626115 DOI: https://doi.org/10.1080/02640414.2019.1626115
Zhang Y, Yang L. Exercise training as an adjunctive therapy to montelukast in children with mild asthma. Medicine. 2019;98(2):e14046. https://doi.org/10.1097/MD.0000000000014046 DOI: https://doi.org/10.1097/MD.0000000000014046
Sanz‐Santiago V, Diez‐Vega I, Santana‐Sosa E, Nuevo CL, Ramirez TI, Vendrusculo FM, et al. Effect of a combined exercise program on physical fitness, lung function, and quality of life in patients with controlled asthma and exercise symptoms: A randomized controlled trial. Pediatr Pulmonol. 2020;55(7):1608-16. https://doi.org/10.1002/ppul.24798 DOI: https://doi.org/10.1002/ppul.24798
Muehlbauer T, Gollhofer A, Granacher U. Associations between measures of balance and lower-extremity muscle strength/power in healthy individuals across the lifespan: a systematic review and meta-analysis. Sports Med. 2015;45(12):1671-92. https://doi.org/10.1007/s40279-015-0390-z DOI: https://doi.org/10.1007/s40279-015-0390-z
Locquet M, Beaudart C, Durieux N, Reginster JY, Bruyère O. Relationship between the changes over time of bone mass and muscle health in children and adults: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20:429. https://doi.org/10.1186/s12891-019-2752-4 DOI: https://doi.org/10.1186/s12891-019-2752-4
Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. https://doi.org/10.1186/1479-5868-7-40 DOI: https://doi.org/10.1186/1479-5868-7-40
Villa F, Castro APBM, Pastorino AC, Santarém JM, Martins MA, Jacob CMA, at el. Aerobic capacity and skeletal muscle function in children with asthma. Arch Dis Child. 2011;96(6):554-9. https://doi.org/10.1136/adc.2011.212431 DOI: https://doi.org/10.1136/adc.2011.212431
França-Pinto A, Mendes FAR, Carvalho-Pinto RM, Agondi RC, Cukier A, Stelmach R, et al. Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: a randomized controlled trial. Thorax. 2015;70:732 9. https://doi.org/10.1136/thoraxjnl-2014-206070 DOI: https://doi.org/10.1136/thoraxjnl-2014-206070
Zhang W, Wang Q, Liu L, Yang W, Liu H. Effects of physical therapy on lung function in children with asthma: a systematic review and meta-analysis. Pediatr Res. 2021;89:1343-51. https://doi.org/10.1038/s41390-020-0874-x DOI: https://doi.org/10.1038/s41390-020-0874-x
Vogiatzis I, Zakynthinos G, Andrianopoulos V. Mechanisms of physical activity limitation in chronic lung diseases. Pulm Med. 2012;2012:634761. https://doi.org/10.1155/2012/634761 DOI: https://doi.org/10.1155/2012/634761
Moraes EZC, Trevisan ME, Baldisserotto SV, Portela LOC. Capacidade aeróbica em crianças e adolescentes com asma intermitente e persistente leve no período intercrises. J Bras Pneumol. 2012;38(4):438-44. https://doi.org/10.1590/S1806-37132012000400005 DOI: https://doi.org/10.1590/S1806-37132012000400005
Júnior DRSA, Souza RB, Santos SA, Andrade DR. Os radicais livres de oxigênio e as doenças pulmonares. J Bras Pneumol. 2005;31(1):60-8. https://doi.org/10.1590/S1806-37132005000100011 DOI: https://doi.org/10.1590/S1806-37132005000100011
Sahiner UM, Birben E, Erzurum S, Sackesen C, Kalayci O. Oxidative stress in asthma. World Allergy Organ J. 2011;4(10):151-8. https://doi.org/10.1097/WOX.0b013e318232389e DOI: https://doi.org/10.1097/WOX.0b013e318232389e
Constantino GTL, Mello Jr JF. Remodelamento das vias aéreas inferiores e superiores. Rev Bras Otorrinolaringol. 2009;75(1):151-6. https://doi.org/10.1590/S0034-72992009000100024 DOI: https://doi.org/10.1590/S0034-72992009000100024
Pawankar R. Perspectivas atuais sobre inflamação e remodelamento das vias aéreas na asma e na rinite alérgica. Braz J Allergy Immunol. 2013 [cited 2022 Feb24];1(5):243-252. Avaiable from: https://bit.ly/36Ew7Br
La Scala CS, Naspitz CK, Solé D. Adaptation and validation of the Pediatric Asthma Quality of Life Questionnaire (PAQLQ) in Brazilian asthmatic children and adolescents. J Pediatr (Rio J), 2005;81:54-60. https://doi.org/10.2223/1283 DOI: https://doi.org/10.2223/1283
Annett RD. Assessment of health status and quality of life outcomes for children with asthma. J Allergy Clin Immunol. 2001;107(5):S473-81. https://doi.org/10.1067/mai.2001.114949 DOI: https://doi.org/10.1067/mai.2001.114949
Everhart RS, Fiese BH. Asthma severity and child quality of life in pediatric asthma: A systematic review. Patient Educ Couns. 2009;75(2):162-8. https://doi.org/10.1016/j.pec.2008.10.001 DOI: https://doi.org/10.1016/j.pec.2008.10.001
Matsunaga NY, Ribeiro MAGO, Saad IAB, Morcillo AM, Ribeiro JD, Toro AADC. Evaluation of quality of life according to asthma control and asthma severity in children and adolescents. J Bras Pneumol. 2015;41(6):502-8. https://doi.org/10.1590/s1806-37562015000000186 DOI: https://doi.org/10.1590/s1806-37562015000000186
Leal RCAC, Braile DM, Souza DRS, Batigália F. Modelo assistencial para pacientes com asma na atenção primária. Rev Assoc Med Bras. 2011;57(6):697-701. https://doi.org/10.1590/S0104-42302011000600019 DOI: https://doi.org/10.1590/S0104-42302011000600019