Intestinal Microbiota and Sclerosis Lateral Amyotrophic
Main Article Content
Abstract
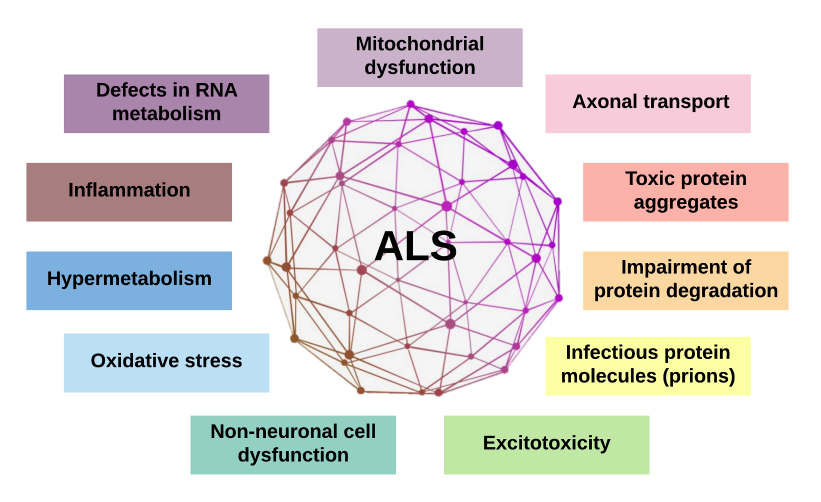
The human gastrointestinal tract contains numerous microorganisms. This intestinal microbiota (IM) has a mutualistic relationship with the human organism, and it plays a fundamental role in regulating metabolic, endocrine, and immunological functions. Intestinal dysbiosis is associated with phenotypes of many chronic and inflammatory diseases. This association is explained by the functions of the IM and the existing bi-directional communication of the microbiota-intestine-brain axis. Studies have uncovered new evidence between the IM and neurodegenerative diseases recently, including amyotrophic lateral sclerosis (ALS). Given this, the present narrative review discusses didactically about IM, its functions, its relationship with the neuroimmune-endocrine system, and its association with neurodegenerative diseases, with emphasis on ALS.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Kho ZY, Lal SK. The human gut microbiome - a potential controller of wellness and disease. Front Microbiol. 2018;9:1835. https://doi.org/10.3389/fmicb.2018.01835 DOI: https://doi.org/10.3389/fmicb.2018.01835
Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13(4):260-70. https://doi.org/10.1038/nrg3182 DOI: https://doi.org/10.1038/nrg3182
McCombe PA, Henderson RD, Lee A, Lee JD, Woodruff TM, Restuadi R, et al. Gut microbiota in ALS: possible role in pathogenesis? Expert Rev Neurother. 2019;19(9):785-805. https://doi.org/10.1080/14737175.2019.1623026 DOI: https://doi.org/10.1080/14737175.2019.1623026
Dinan TG, Cryan JF. The microbiome-gut-brain axis in health and disease. Gastroenterol Clin N Am. 2017;46:77-89. https://doi.org/10.1016/j.gtc.2016.09.007 DOI: https://doi.org/10.1016/j.gtc.2016.09.007
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14(8):e1002533. https://doi.org/10.1371/journal.pbio.1002533 DOI: https://doi.org/10.1371/journal.pbio.1002533
Ding RX, Goh WR, Wu RN, Yue XQ, Luo X, Khine WWT, et al. Revisit gut microbiota and its impact on human health and disease. J Food Drug Anal. 2019;27(3):623-31. https://doi.org/10.1016/j.jfda.2018.12.012 DOI: https://doi.org/10.1016/j.jfda.2018.12.012
Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, et al. What is the healthy gut microbiota composition? A Changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019;7(1):14. https://doi.org/10.3390/microorganisms7010014 DOI: https://doi.org/10.3390/microorganisms7010014
Mariat D, Firmesse O, Levenez F, Guimarăes V, Sokol H, Doré J, et al. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009;9:123. https://doi.org/10.1186/1471-2180-9-123 DOI: https://doi.org/10.1186/1471-2180-9-123
Clarke G, Sandhu KV, Griffin BT, Dinan TG, Cryan JF, Hyland NP. Gut Reactions: Breaking down xenobiotic-microbiome interactions. Pharmacol Rev. 2019;71(2):198-224. https://doi.org/10.1124/pr.118.015768 DOI: https://doi.org/10.1124/pr.118.015768
Selma-Royo M, Tarrazó M, García-Mantrana I, Gómez-Gallego C, Salminen S, Collado MC. Shaping microbiota during the first 1000 days of life. Adv Exp Med Biol. 2019;1125:3-24. https://doi.org/10.1007/5584_2018_312 DOI: https://doi.org/10.1007/5584_2018_312
Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. 2017;81(4):e00036-17. https://doi.org/10.1128/MMBR.00036-17 DOI: https://doi.org/10.1128/MMBR.00036-17
Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017;474(11):1823-36. https://doi.org/10.1042/BCJ20160510 DOI: https://doi.org/10.1042/BCJ20160510
den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54(9):2325-40. https://doi.org/10.1194/jlr.R036012 DOI: https://doi.org/10.1194/jlr.R036012
Venegas DP, la Fuente MK, Landskron G, González MJ, Quera R, Dijkstra G, et al. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;20:277. https://doi.org/10.3389/fimmu.2019.00277 DOI: https://doi.org/10.3389/fimmu.2019.00277
Amoroso C, Perillo F, Strati F, Fantini MC, Caprioli F, Facciotti F. The role of gut microbiota biomodulators on mucosal immunity and intestinal inflammation. Cells. 2020;9(5):1234. https://doi.org/10.3390/cells9051234 DOI: https://doi.org/10.3390/cells9051234
Yadav M, Verma MK, Chauhan NS. A review of metabolic potential of human gut microbiome in human nutrition. Arch Microbiol. 2018;200(2):203-17. https://doi.org/10.1007/s00203-017-1459-x DOI: https://doi.org/10.1007/s00203-017-1459-x
Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91-119. https://doi.org/10.1016/B978-0-12-800100-4.00003-9 DOI: https://doi.org/10.1016/B978-0-12-800100-4.00003-9
Liu H, Wang J, He T, Becker S, Zhang G, Li D, et al. Butyrate: A double-edged sword for health? Adv Nutr. 2018;9(1):21-9. https://doi.org/10.1093/advances/nmx009 DOI: https://doi.org/10.1093/advances/nmx009
Lin MY, de Zoete MR, van Putten JP, Strijbis K. Redirection of epithelial immune responses by short-chain fatty acids through inhibition of histone deacetylases. Front Immunol. 2015;6:554. https://doi.org/10.3389/fimmu.2015.00554 DOI: https://doi.org/10.3389/fimmu.2015.00554
Li M, van Esch BCAM, Henricks PAJ, Folkerts G, Garssen J. The anti-inflammatory effects of short chain fatty acids on lipopolysaccharide- or tumor necrosis factor α-stimulated endothelial cells via activation of GPR41/43 and inhibition of HDACs. Front Pharmacol. 2018;9:533. https://doi.org/10.3389/fphar.2018.00533 DOI: https://doi.org/10.3389/fphar.2018.00533
Yang G, Chen S, Deng B, Tan C, Deng J, Zhu G, et al. Implication of G protein-coupled receptor 43 in intestinal inflammation: a mini-review. Front Immunol. 2018;9:1434. https://doi.org/10.3389/fimmu.2018.01434 DOI: https://doi.org/10.3389/fimmu.2018.01434
Tazoe H, Otomo Y, Kaji I, Tanaka R, Karaki SI, Kuwahara A. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J Physiol Pharmacol. 2008;59 (Suppl 2):251-62. PMID: 18812643
Gaboriau-Routhiau V, Rakotobe S, Lécuyer E, Mulder I, Lan A, Bridonneau C, et al. The key role of segmented filamentous bacteria in the coordinated maturation of gut helper T cell responses. Immunity. 2009;31(4):677-689. https://doi.org/10.1016/j.immuni.2009.08.020 DOI: https://doi.org/10.1016/j.immuni.2009.08.020
Marietta E, Horwath I, Taneja V. Microbiome, immunomodulation, and the neuronal system. Neurotherapeutics. 2018;15:23-30. https://doi.org/10.1007/s13311-017-0601-4 DOI: https://doi.org/10.1007/s13311-017-0601-4
Corrêa-Oliveira R, Fachi JL, Vieira A, Sato FT, Vinolo MA. Regulation of immune cell function by short-chain fatty acids. Clin Transl Immunology. 2016;5(4):e73. https://doi.org/10.1038/cti.2016.17 DOI: https://doi.org/10.1038/cti.2016.17
Wang HX; Wang YP. Gut microbiota-brain axis. Chin Med J. 2016;129(19):2372-2380. https://doi.org/10.4103/0366-6999.190667 DOI: https://doi.org/10.4103/0366-6999.190667
Gagliardi A, Totino V, Cacciotti F, Iebba V, Neroni B, Bonfiglio G, et al. Rebuilding the gut microbiota ecosystem. Int J Environ Res Public Health. 2018;15(8):1679. https://doi.org/10.3390/ijerph15081679 DOI: https://doi.org/10.3390/ijerph15081679
Benakis C, Martin-Gallausiaux C, Trezzi JP, Melton P, Liesz A, Wilmes P. The microbiome-gut-brain axis in acute and chronic brain diseases. Curr Opin Neurobiol. 2020;61:1-9. https://doi.org/10.1016/j.conb.2019.11.009 DOI: https://doi.org/10.1016/j.conb.2019.11.009
Sasmita AO. Modification of the gut microbiome to combat neurodegeneration. Rev. Neurosci. 2019;30:795-805. https://doi.org/10.1515/revneuro-2019-0005 DOI: https://doi.org/10.1515/revneuro-2019-0005
Di Gioia D, Cionci NB, Baffoni L, Amoruso A, Pane M, Mogna L, et al. A prospective longitudinal study on the microbiota composition in amyotrophic lateral sclerosis. BMC Med. 2020;18(1):153. https://doi.org/10.1186/s12916-020-01607-9 DOI: https://doi.org/10.1186/s12916-020-01607-9
van Es MA, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp RJ, Veldink JH, et al. Amyotrophic lateral sclerosis. Lancet. 2017;390(10107):2084-98. https://doi.org/10.1016/S0140-6736(17)31287-4 DOI: https://doi.org/10.1016/S0140-6736(17)31287-4
Gois AM, Mendonça DMF, Freire MAM, Santos JR. In vitro and in vivo models of amyotrophic lateral sclerosis: an updated overview. Brain Res Bull. 2020;159:32-43. https://doi.org/10.1016/j.brainresbull.2020.03.012 DOI: https://doi.org/10.1016/j.brainresbull.2020.03.012
Bonifacino T, Zerbo RA, Balbi M, Torazza C, Frumento G, Fedele E, et al. Nearly 30 years of animal models to study amyotrophic lateral sclerosis: a historical overview and future perspectives. Int J Mol Sci. 2021;22(22):12236. https://doi.org/10.3390/ijms222212236 DOI: https://doi.org/10.3390/ijms222212236
Wu S, Yi J, Zhang YG, Zhou J, Sun J. Leaky intestine and impaired microbiome in an amyotrophic lateral sclerosis mouse model. Physiol Rep. 2015;3(4):e12356. https://doi.org/10.14814/phy2.12356 DOI: https://doi.org/10.14814/phy2.12356
Fang X, Wang X, Yang S, Meng F, Wang X, Wei H, et al. Evaluation of the microbial diversity in amyotrophic lateral sclerosis using high-throughput sequencing. Front Microbiol. 2016;7:1479. https://doi.org/10.3389/fmicb.2016.01479 DOI: https://doi.org/10.3389/fmicb.2016.01479
Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health? Neurosci Lett. 2016;625:56-63. https://doi.org/10.1016/j.neulet.2016.02.009 DOI: https://doi.org/10.1016/j.neulet.2016.02.009
Huuskonen J, Suuronen T, Nuutinen T, Kyrylenko S, Salminen A. Regulation of microglial inflammatory response by sodium butyrate and short-chain fatty acids. Br J Pharmacol. 2004;141(5):874-80. https://doi.org/10.1038/sj.bjp.0705682 DOI: https://doi.org/10.1038/sj.bjp.0705682
Ryu H, Smith K, Camelo SI, Carreras I, Lee J, Iglesias AH, et al. Sodium phenylbutyrate prolongs survival and regulates expression of anti-apoptotic genes in transgenic amyotrophic lateral sclerosis mice. J Neurochem. 2005;93(5):1087-98. https://doi.org/10.1111/j.1471-4159.2005.03077.x DOI: https://doi.org/10.1111/j.1471-4159.2005.03077.x
Zhang YG, Wu S, Yi J, Xia Y, Jin D, Zhou J, et al. Target intestinal microbiota to alleviate disease progression in amyotrophic lateral sclerosis. Clin Ther. 2017;39(2):322-36. https://doi.org/10.1016/j.clinthera.2016.12.014 DOI: https://doi.org/10.1016/j.clinthera.2016.12.014
Cudkowicz ME, Andres PL, Macdonald SA, Bedlack RS, Choudry R, Brown Jr. RH, et al. Phase 2 study of sodium phenylbutyrate in ALS. Amyotroph Lateral Scler. 2009;10(2):99-106. https://doi.org/10.1080/17482960802320487 DOI: https://doi.org/10.1080/17482960802320487
Paganoni S, Macklin EA, Hendrix S, Berry JD, Elliott MA, Maiser S, et al. Trial of sodium phenylbutyrate-taurursodiol for amyotrophic lateral sclerosis. N Engl J Med. 2020;383(10):919-30. https://doi.org/10.1056/NEJMoa1916945 DOI: https://doi.org/10.1056/NEJMoa1916945
Wright ML, Fournier C, Houser MC, Tansey M, Glass J, Hertzberg VS. Potential role of the gut microbiome in ALS: a systematic review. Biol Res Nurs. 2018;20(5):513-21. https://doi.org/10.1177/1099800418784202 DOI: https://doi.org/10.1177/1099800418784202
Cai M, Yang EJ. Complementary and alternative medicine for treating amyotrophic lateral sclerosis: A narrative review. Integr Med Res. 2019;8(4):234-9. https://doi.org/10.1016/j.imr.2019.08.003 DOI: https://doi.org/10.1016/j.imr.2019.08.003
Nieves JW, Gennings C, Factor-Litvak P, Hupf J, Singleton J, Sharf V, et al. Association between dietary intake and function in amyotrophic lateral sclerosis. JAMA Neurol. 2016;73(12):1425-32. https://doi.org/10.1001/jamaneurol.2016.3401 DOI: https://doi.org/10.1001/jamaneurol.2016.3401
Wills AM, Hubbard J, Macklin EA, Glass J, Tandan R, Simpson EP, et al. Hypercaloric enteral nutrition in patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet. 2014;383(9934):2065-72. https://doi.org/10.1016/S0140-6736(14)60222-1 DOI: https://doi.org/10.1016/S0140-6736(14)60222-1
Heiman ML, Greenway FL. A healthy gastrointestinal microbiome is dependent on dietary diversity. Mol Metab. 2016;5(5):317-20. https://doi.org/10.1016/j.molmet.2016.02.005 DOI: https://doi.org/10.1016/j.molmet.2016.02.005
Markowiak P, Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9(9):1021. https://doi.org/10.3390/nu9091021 DOI: https://doi.org/10.3390/nu9091021
Guarner F, Khan AG, Garisch J, Eliakim R, Gangl A, Thomson A, et al. World Gastroenterology Organisation Global Guidelines - Probiotics and Prebiotics. World Gastroenterology Organisation, 2017. 35p. https://doi.org/10.1097/MCG.0b013e3182549092 DOI: https://doi.org/10.1097/MCG.0b013e3182549092
Maguire M, Maguire G. Gut dysbiosis, leaky gut, and intestinal epithelial proliferation in neurological disorders: towards the development of a new therapeutic using amino acids, prebiotics, probiotics, and postbiotics. Rev Neurosci. 2019;30(2):179-201. https://doi.org/10.1515/revneuro-2018-0024 DOI: https://doi.org/10.1515/revneuro-2018-0024
Kuraszkiewicz B, Goszczyńska H, Podsiadły-Marczykowska T, Piotrkiewicz M, Andersen P, Gromicho M, et al. Potential Preventive Strategies for Amyotrophic Lateral Sclerosis. Front Neurosci. 2020;14:428. https://doi.org/10.3389/fnins.2020.00428 DOI: https://doi.org/10.3389/fnins.2020.00428
Liscic RM, Alberici A, Cairns NJ, Romano M, Buratti E. From basic research to the clinic: innovative therapies for ALS and FTD in the pipeline. Mol Neurodegener. 2020;15(1):31. https://doi.org/10.1186/s13024-020-00373-9 DOI: https://doi.org/10.1186/s13024-020-00373-9
Sniffen JC, McFarland LV, Evans CT, Goldstein EJC. Choosing an appropriate probiotic product for your patient: An evidence-based practical guide. PLoS One. 2018;13(12):e0209205. https://doi.org/10.1371/journal.pone.0209205 DOI: https://doi.org/10.1371/journal.pone.0209205
Russo E, Giudici F, Fiorindi C, Ficari F, Scaringi S, Amedei A. immunomodulating activity and therapeutic effects of short chain fatty acids and tryptophan post-biotics in inflammatory bowel disease. Front Immunol. 2019;10:2754. https://doi.org/10.3389/fimmu.2019.02754 DOI: https://doi.org/10.3389/fimmu.2019.02754
Wang W, Zhao J, Gui W, Sun D, Dai H, Xiao L, et al. Tauroursodeoxycholic acid inhibits intestinal inflammation and barrier disruption in mice with non-alcoholic fatty liver disease. Br J Pharmacol. 2018;175(3):469-84. https://doi.org/10.1111/bph.14095 DOI: https://doi.org/10.1111/bph.14095
Daruich A, Picard E, Boatright JH, Behar-Cohen F. Review: The bile acids urso- and tauroursodeoxycholic acid as neuroprotective therapies in retinal disease. Mol Vis. 2019;25:610-24. PMCID: PMC6817734
Elia AE, Lalli S, Monsurrò MR, Sagnelli A, Taiello AC, Reggiori B, et al. Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis. Eur J Neurol. 2016;23(1):45-52. https://doi.org/10.1111/ene.12664 DOI: https://doi.org/10.1111/ene.12664
Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958;44:854-9. PMID:13592638
van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-15 https://doi.org/10.1056/NEJMoa1205037 DOI: https://doi.org/10.1056/NEJMoa1205037
Leshem A, Horesh N, Elinav E. Fecal Microbial Transplantation and its potential application in cardiometabolic syndrome. Front Immunol. 2019;10:1341. https://doi.org/10.3389/fimmu.2019.01341 DOI: https://doi.org/10.3389/fimmu.2019.01341
Tilocca B, Pieroni L, Soggiu A, Britti D, Bonizzi L, Roncada P, et al. Gut-brain axis and neurodegeneration: state-of-the-art of meta-omics sciences for microbiota characterization. Int J Mol Sci. 2020;21(11):4045. https://doi.org/10.3390/ijms21114045 DOI: https://doi.org/10.3390/ijms21114045
Vendrik KEW, Ooijevaar RE, de Jong PRC, Laman JD, van Oosten BW, van Hilten JJ, et al. Fecal microbiota transplantation in neurological disorders. Front Cell Infect Microbiol. 2020;10:98. https://doi.org/10.3389/fcimb.2020.00098 DOI: https://doi.org/10.3389/fcimb.2020.00098
Mandrioli J, Amedei A, Cammarota G, Niccolai E, Zucchi E, D'Amico R, et al. FETR-ALS Study Protocol: A randomized clinical trial of fecal microbiota transplantation in amyotrophic lateral sclerosis. Front Neurol. 2019;10:1021. https://doi.org/10.3389/fneur.2019.01021 DOI: https://doi.org/10.3389/fneur.2019.01021