Microbiota Intestinal e Esclerose Lateral Amiotrófica
Conteúdo do artigo principal
Resumo
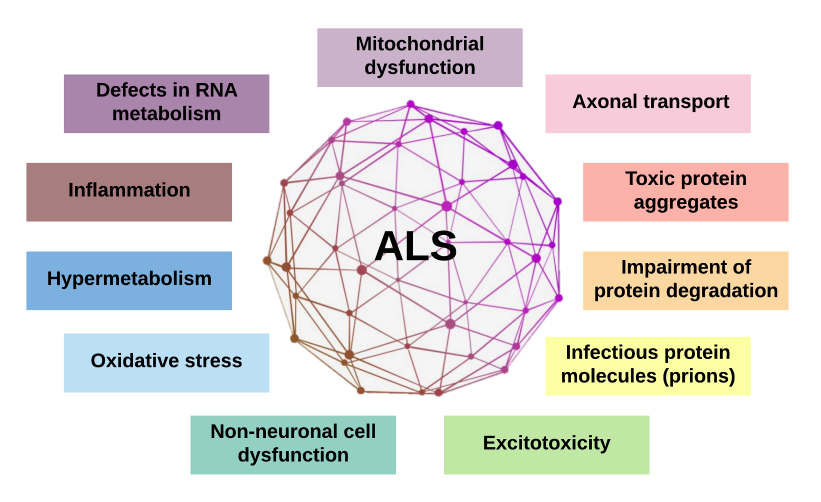
O trato gastrintestinal humano é povoado por uma grande quantidade de microrganismos. Essa microbiota intestinal (MI) tem uma relação de mutualismo com o organismo humano e desempenha papel fundamental na regulação de funções metabólicas, endócrinas e imunológicas. A disbiose intestinal está associada a fenótipos de várias doenças crônicas e inflamatórias. Essa associação é explicada pelas funções da MI e a existente comunicação bidirecional do eixo microbiota-intestino-cérebro. Nos últimos anos, estudos têm mostrado novas evidências entre a MI e as doenças neurodegenerativas, incluindo a esclerose lateral amiotrófica (ELA). Diante disso, essa revisão narrativa discorre de forma didática sobre a MI, suas funções, sua relação com o sistema neuro-imuno-endócrino e sua associação com as doenças neurodegenerativas, com ênfase na ELA.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
Kho ZY, Lal SK. The human gut microbiome - a potential controller of wellness and disease. Front Microbiol. 2018;9:1835. https://doi.org/10.3389/fmicb.2018.01835 DOI: https://doi.org/10.3389/fmicb.2018.01835
Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13(4):260-70. https://doi.org/10.1038/nrg3182 DOI: https://doi.org/10.1038/nrg3182
McCombe PA, Henderson RD, Lee A, Lee JD, Woodruff TM, Restuadi R, et al. Gut microbiota in ALS: possible role in pathogenesis? Expert Rev Neurother. 2019;19(9):785-805. https://doi.org/10.1080/14737175.2019.1623026 DOI: https://doi.org/10.1080/14737175.2019.1623026
Dinan TG, Cryan JF. The microbiome-gut-brain axis in health and disease. Gastroenterol Clin N Am. 2017;46:77-89. https://doi.org/10.1016/j.gtc.2016.09.007 DOI: https://doi.org/10.1016/j.gtc.2016.09.007
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14(8):e1002533. https://doi.org/10.1371/journal.pbio.1002533 DOI: https://doi.org/10.1371/journal.pbio.1002533
Ding RX, Goh WR, Wu RN, Yue XQ, Luo X, Khine WWT, et al. Revisit gut microbiota and its impact on human health and disease. J Food Drug Anal. 2019;27(3):623-31. https://doi.org/10.1016/j.jfda.2018.12.012 DOI: https://doi.org/10.1016/j.jfda.2018.12.012
Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, et al. What is the healthy gut microbiota composition? A Changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019;7(1):14. https://doi.org/10.3390/microorganisms7010014 DOI: https://doi.org/10.3390/microorganisms7010014
Mariat D, Firmesse O, Levenez F, Guimarăes V, Sokol H, Doré J, et al. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009;9:123. https://doi.org/10.1186/1471-2180-9-123 DOI: https://doi.org/10.1186/1471-2180-9-123
Clarke G, Sandhu KV, Griffin BT, Dinan TG, Cryan JF, Hyland NP. Gut Reactions: Breaking down xenobiotic-microbiome interactions. Pharmacol Rev. 2019;71(2):198-224. https://doi.org/10.1124/pr.118.015768 DOI: https://doi.org/10.1124/pr.118.015768
Selma-Royo M, Tarrazó M, García-Mantrana I, Gómez-Gallego C, Salminen S, Collado MC. Shaping microbiota during the first 1000 days of life. Adv Exp Med Biol. 2019;1125:3-24. https://doi.org/10.1007/5584_2018_312 DOI: https://doi.org/10.1007/5584_2018_312
Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. 2017;81(4):e00036-17. https://doi.org/10.1128/MMBR.00036-17 DOI: https://doi.org/10.1128/MMBR.00036-17
Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017;474(11):1823-36. https://doi.org/10.1042/BCJ20160510 DOI: https://doi.org/10.1042/BCJ20160510
den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54(9):2325-40. https://doi.org/10.1194/jlr.R036012 DOI: https://doi.org/10.1194/jlr.R036012
Venegas DP, la Fuente MK, Landskron G, González MJ, Quera R, Dijkstra G, et al. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;20:277. https://doi.org/10.3389/fimmu.2019.00277 DOI: https://doi.org/10.3389/fimmu.2019.00277
Amoroso C, Perillo F, Strati F, Fantini MC, Caprioli F, Facciotti F. The role of gut microbiota biomodulators on mucosal immunity and intestinal inflammation. Cells. 2020;9(5):1234. https://doi.org/10.3390/cells9051234 DOI: https://doi.org/10.3390/cells9051234
Yadav M, Verma MK, Chauhan NS. A review of metabolic potential of human gut microbiome in human nutrition. Arch Microbiol. 2018;200(2):203-17. https://doi.org/10.1007/s00203-017-1459-x DOI: https://doi.org/10.1007/s00203-017-1459-x
Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91-119. https://doi.org/10.1016/B978-0-12-800100-4.00003-9 DOI: https://doi.org/10.1016/B978-0-12-800100-4.00003-9
Liu H, Wang J, He T, Becker S, Zhang G, Li D, et al. Butyrate: A double-edged sword for health? Adv Nutr. 2018;9(1):21-9. https://doi.org/10.1093/advances/nmx009 DOI: https://doi.org/10.1093/advances/nmx009
Lin MY, de Zoete MR, van Putten JP, Strijbis K. Redirection of epithelial immune responses by short-chain fatty acids through inhibition of histone deacetylases. Front Immunol. 2015;6:554. https://doi.org/10.3389/fimmu.2015.00554 DOI: https://doi.org/10.3389/fimmu.2015.00554
Li M, van Esch BCAM, Henricks PAJ, Folkerts G, Garssen J. The anti-inflammatory effects of short chain fatty acids on lipopolysaccharide- or tumor necrosis factor α-stimulated endothelial cells via activation of GPR41/43 and inhibition of HDACs. Front Pharmacol. 2018;9:533. https://doi.org/10.3389/fphar.2018.00533 DOI: https://doi.org/10.3389/fphar.2018.00533
Yang G, Chen S, Deng B, Tan C, Deng J, Zhu G, et al. Implication of G protein-coupled receptor 43 in intestinal inflammation: a mini-review. Front Immunol. 2018;9:1434. https://doi.org/10.3389/fimmu.2018.01434 DOI: https://doi.org/10.3389/fimmu.2018.01434
Tazoe H, Otomo Y, Kaji I, Tanaka R, Karaki SI, Kuwahara A. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J Physiol Pharmacol. 2008;59 (Suppl 2):251-62. PMID: 18812643
Gaboriau-Routhiau V, Rakotobe S, Lécuyer E, Mulder I, Lan A, Bridonneau C, et al. The key role of segmented filamentous bacteria in the coordinated maturation of gut helper T cell responses. Immunity. 2009;31(4):677-689. https://doi.org/10.1016/j.immuni.2009.08.020 DOI: https://doi.org/10.1016/j.immuni.2009.08.020
Marietta E, Horwath I, Taneja V. Microbiome, immunomodulation, and the neuronal system. Neurotherapeutics. 2018;15:23-30. https://doi.org/10.1007/s13311-017-0601-4 DOI: https://doi.org/10.1007/s13311-017-0601-4
Corrêa-Oliveira R, Fachi JL, Vieira A, Sato FT, Vinolo MA. Regulation of immune cell function by short-chain fatty acids. Clin Transl Immunology. 2016;5(4):e73. https://doi.org/10.1038/cti.2016.17 DOI: https://doi.org/10.1038/cti.2016.17
Wang HX; Wang YP. Gut microbiota-brain axis. Chin Med J. 2016;129(19):2372-2380. https://doi.org/10.4103/0366-6999.190667 DOI: https://doi.org/10.4103/0366-6999.190667
Gagliardi A, Totino V, Cacciotti F, Iebba V, Neroni B, Bonfiglio G, et al. Rebuilding the gut microbiota ecosystem. Int J Environ Res Public Health. 2018;15(8):1679. https://doi.org/10.3390/ijerph15081679 DOI: https://doi.org/10.3390/ijerph15081679
Benakis C, Martin-Gallausiaux C, Trezzi JP, Melton P, Liesz A, Wilmes P. The microbiome-gut-brain axis in acute and chronic brain diseases. Curr Opin Neurobiol. 2020;61:1-9. https://doi.org/10.1016/j.conb.2019.11.009 DOI: https://doi.org/10.1016/j.conb.2019.11.009
Sasmita AO. Modification of the gut microbiome to combat neurodegeneration. Rev. Neurosci. 2019;30:795-805. https://doi.org/10.1515/revneuro-2019-0005 DOI: https://doi.org/10.1515/revneuro-2019-0005
Di Gioia D, Cionci NB, Baffoni L, Amoruso A, Pane M, Mogna L, et al. A prospective longitudinal study on the microbiota composition in amyotrophic lateral sclerosis. BMC Med. 2020;18(1):153. https://doi.org/10.1186/s12916-020-01607-9 DOI: https://doi.org/10.1186/s12916-020-01607-9
van Es MA, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp RJ, Veldink JH, et al. Amyotrophic lateral sclerosis. Lancet. 2017;390(10107):2084-98. https://doi.org/10.1016/S0140-6736(17)31287-4 DOI: https://doi.org/10.1016/S0140-6736(17)31287-4
Gois AM, Mendonça DMF, Freire MAM, Santos JR. In vitro and in vivo models of amyotrophic lateral sclerosis: an updated overview. Brain Res Bull. 2020;159:32-43. https://doi.org/10.1016/j.brainresbull.2020.03.012 DOI: https://doi.org/10.1016/j.brainresbull.2020.03.012
Bonifacino T, Zerbo RA, Balbi M, Torazza C, Frumento G, Fedele E, et al. Nearly 30 years of animal models to study amyotrophic lateral sclerosis: a historical overview and future perspectives. Int J Mol Sci. 2021;22(22):12236. https://doi.org/10.3390/ijms222212236 DOI: https://doi.org/10.3390/ijms222212236
Wu S, Yi J, Zhang YG, Zhou J, Sun J. Leaky intestine and impaired microbiome in an amyotrophic lateral sclerosis mouse model. Physiol Rep. 2015;3(4):e12356. https://doi.org/10.14814/phy2.12356 DOI: https://doi.org/10.14814/phy2.12356
Fang X, Wang X, Yang S, Meng F, Wang X, Wei H, et al. Evaluation of the microbial diversity in amyotrophic lateral sclerosis using high-throughput sequencing. Front Microbiol. 2016;7:1479. https://doi.org/10.3389/fmicb.2016.01479 DOI: https://doi.org/10.3389/fmicb.2016.01479
Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health? Neurosci Lett. 2016;625:56-63. https://doi.org/10.1016/j.neulet.2016.02.009 DOI: https://doi.org/10.1016/j.neulet.2016.02.009
Huuskonen J, Suuronen T, Nuutinen T, Kyrylenko S, Salminen A. Regulation of microglial inflammatory response by sodium butyrate and short-chain fatty acids. Br J Pharmacol. 2004;141(5):874-80. https://doi.org/10.1038/sj.bjp.0705682 DOI: https://doi.org/10.1038/sj.bjp.0705682
Ryu H, Smith K, Camelo SI, Carreras I, Lee J, Iglesias AH, et al. Sodium phenylbutyrate prolongs survival and regulates expression of anti-apoptotic genes in transgenic amyotrophic lateral sclerosis mice. J Neurochem. 2005;93(5):1087-98. https://doi.org/10.1111/j.1471-4159.2005.03077.x DOI: https://doi.org/10.1111/j.1471-4159.2005.03077.x
Zhang YG, Wu S, Yi J, Xia Y, Jin D, Zhou J, et al. Target intestinal microbiota to alleviate disease progression in amyotrophic lateral sclerosis. Clin Ther. 2017;39(2):322-36. https://doi.org/10.1016/j.clinthera.2016.12.014 DOI: https://doi.org/10.1016/j.clinthera.2016.12.014
Cudkowicz ME, Andres PL, Macdonald SA, Bedlack RS, Choudry R, Brown Jr. RH, et al. Phase 2 study of sodium phenylbutyrate in ALS. Amyotroph Lateral Scler. 2009;10(2):99-106. https://doi.org/10.1080/17482960802320487 DOI: https://doi.org/10.1080/17482960802320487
Paganoni S, Macklin EA, Hendrix S, Berry JD, Elliott MA, Maiser S, et al. Trial of sodium phenylbutyrate-taurursodiol for amyotrophic lateral sclerosis. N Engl J Med. 2020;383(10):919-30. https://doi.org/10.1056/NEJMoa1916945 DOI: https://doi.org/10.1056/NEJMoa1916945
Wright ML, Fournier C, Houser MC, Tansey M, Glass J, Hertzberg VS. Potential role of the gut microbiome in ALS: a systematic review. Biol Res Nurs. 2018;20(5):513-21. https://doi.org/10.1177/1099800418784202 DOI: https://doi.org/10.1177/1099800418784202
Cai M, Yang EJ. Complementary and alternative medicine for treating amyotrophic lateral sclerosis: A narrative review. Integr Med Res. 2019;8(4):234-9. https://doi.org/10.1016/j.imr.2019.08.003 DOI: https://doi.org/10.1016/j.imr.2019.08.003
Nieves JW, Gennings C, Factor-Litvak P, Hupf J, Singleton J, Sharf V, et al. Association between dietary intake and function in amyotrophic lateral sclerosis. JAMA Neurol. 2016;73(12):1425-32. https://doi.org/10.1001/jamaneurol.2016.3401 DOI: https://doi.org/10.1001/jamaneurol.2016.3401
Wills AM, Hubbard J, Macklin EA, Glass J, Tandan R, Simpson EP, et al. Hypercaloric enteral nutrition in patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet. 2014;383(9934):2065-72. https://doi.org/10.1016/S0140-6736(14)60222-1 DOI: https://doi.org/10.1016/S0140-6736(14)60222-1
Heiman ML, Greenway FL. A healthy gastrointestinal microbiome is dependent on dietary diversity. Mol Metab. 2016;5(5):317-20. https://doi.org/10.1016/j.molmet.2016.02.005 DOI: https://doi.org/10.1016/j.molmet.2016.02.005
Markowiak P, Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9(9):1021. https://doi.org/10.3390/nu9091021 DOI: https://doi.org/10.3390/nu9091021
Guarner F, Khan AG, Garisch J, Eliakim R, Gangl A, Thomson A, et al. World Gastroenterology Organisation Global Guidelines - Probiotics and Prebiotics. World Gastroenterology Organisation, 2017. 35p. https://doi.org/10.1097/MCG.0b013e3182549092 DOI: https://doi.org/10.1097/MCG.0b013e3182549092
Maguire M, Maguire G. Gut dysbiosis, leaky gut, and intestinal epithelial proliferation in neurological disorders: towards the development of a new therapeutic using amino acids, prebiotics, probiotics, and postbiotics. Rev Neurosci. 2019;30(2):179-201. https://doi.org/10.1515/revneuro-2018-0024 DOI: https://doi.org/10.1515/revneuro-2018-0024
Kuraszkiewicz B, Goszczyńska H, Podsiadły-Marczykowska T, Piotrkiewicz M, Andersen P, Gromicho M, et al. Potential Preventive Strategies for Amyotrophic Lateral Sclerosis. Front Neurosci. 2020;14:428. https://doi.org/10.3389/fnins.2020.00428 DOI: https://doi.org/10.3389/fnins.2020.00428
Liscic RM, Alberici A, Cairns NJ, Romano M, Buratti E. From basic research to the clinic: innovative therapies for ALS and FTD in the pipeline. Mol Neurodegener. 2020;15(1):31. https://doi.org/10.1186/s13024-020-00373-9 DOI: https://doi.org/10.1186/s13024-020-00373-9
Sniffen JC, McFarland LV, Evans CT, Goldstein EJC. Choosing an appropriate probiotic product for your patient: An evidence-based practical guide. PLoS One. 2018;13(12):e0209205. https://doi.org/10.1371/journal.pone.0209205 DOI: https://doi.org/10.1371/journal.pone.0209205
Russo E, Giudici F, Fiorindi C, Ficari F, Scaringi S, Amedei A. immunomodulating activity and therapeutic effects of short chain fatty acids and tryptophan post-biotics in inflammatory bowel disease. Front Immunol. 2019;10:2754. https://doi.org/10.3389/fimmu.2019.02754 DOI: https://doi.org/10.3389/fimmu.2019.02754
Wang W, Zhao J, Gui W, Sun D, Dai H, Xiao L, et al. Tauroursodeoxycholic acid inhibits intestinal inflammation and barrier disruption in mice with non-alcoholic fatty liver disease. Br J Pharmacol. 2018;175(3):469-84. https://doi.org/10.1111/bph.14095 DOI: https://doi.org/10.1111/bph.14095
Daruich A, Picard E, Boatright JH, Behar-Cohen F. Review: The bile acids urso- and tauroursodeoxycholic acid as neuroprotective therapies in retinal disease. Mol Vis. 2019;25:610-24. PMCID: PMC6817734
Elia AE, Lalli S, Monsurrò MR, Sagnelli A, Taiello AC, Reggiori B, et al. Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis. Eur J Neurol. 2016;23(1):45-52. https://doi.org/10.1111/ene.12664 DOI: https://doi.org/10.1111/ene.12664
Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958;44:854-9. PMID:13592638
van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-15 https://doi.org/10.1056/NEJMoa1205037 DOI: https://doi.org/10.1056/NEJMoa1205037
Leshem A, Horesh N, Elinav E. Fecal Microbial Transplantation and its potential application in cardiometabolic syndrome. Front Immunol. 2019;10:1341. https://doi.org/10.3389/fimmu.2019.01341 DOI: https://doi.org/10.3389/fimmu.2019.01341
Tilocca B, Pieroni L, Soggiu A, Britti D, Bonizzi L, Roncada P, et al. Gut-brain axis and neurodegeneration: state-of-the-art of meta-omics sciences for microbiota characterization. Int J Mol Sci. 2020;21(11):4045. https://doi.org/10.3390/ijms21114045 DOI: https://doi.org/10.3390/ijms21114045
Vendrik KEW, Ooijevaar RE, de Jong PRC, Laman JD, van Oosten BW, van Hilten JJ, et al. Fecal microbiota transplantation in neurological disorders. Front Cell Infect Microbiol. 2020;10:98. https://doi.org/10.3389/fcimb.2020.00098 DOI: https://doi.org/10.3389/fcimb.2020.00098
Mandrioli J, Amedei A, Cammarota G, Niccolai E, Zucchi E, D'Amico R, et al. FETR-ALS Study Protocol: A randomized clinical trial of fecal microbiota transplantation in amyotrophic lateral sclerosis. Front Neurol. 2019;10:1021. https://doi.org/10.3389/fneur.2019.01021 DOI: https://doi.org/10.3389/fneur.2019.01021