Profile of blood donors in a hemotherapy institution in Midwestern Brazil
Main Article Content
Abstract
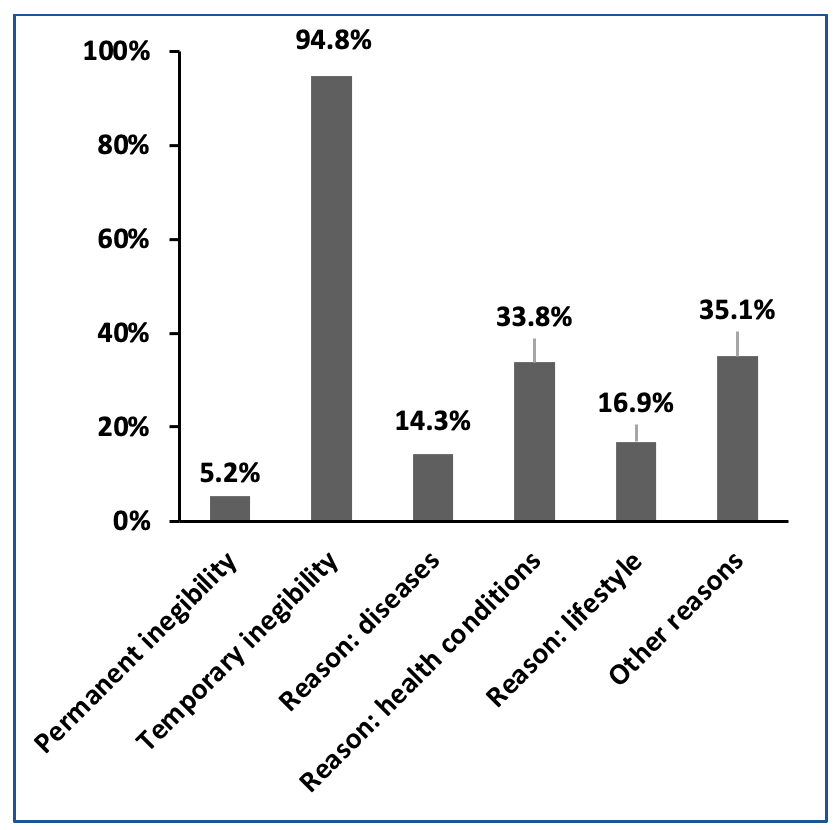
Objective: To describe the profile of blood donors in a hospital in the Midwest of Brazil with its own blood bank to have a diagnostic view of the establishment and enable the planning of improvements in services. Methods: This is a descriptive, retrospective study with a quantitative approach. A proportional stratified sampling technique was used, with a confidence level of 95% and a margin of error of 5%, to represent and characterize the study population, obtaining a sample of 363 donors. Subsequently, a proportional allocation was performed in the established groups (fit donors, unfit donors, and platelet apheresis donors). Results: The profile of eligible donors in the institution studied was composed of married (55.2%), male (63.7%), aged between 20 and 30 years (40.4%), with O RhD+ blood (46.7%) and A RhD+ (29.6%) more prevalent. Apheresis platelet donors (50%) are single, female (81.3%), and aged between 31 and 40 years (43.8%). As for unfit donors, 94.8% are temporary-unfit donors, married donors (53.2%), female (54.5%), and between 20 and 40 years old (54.6%), with the categories of health condition and lifestyle being the most prevalent reasons for disability. Conclusion: There is a hegemony for replacement and first-time donors, showing the effectiveness of the solidarity policy implemented in the institution, but it shows the low effectiveness in the loyalty of these donors.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Amaral JHS, Nunes RLS, Rodrigues LMS, Braz MR, Balbino CM, Silvino ZR. Hemoterapia: um desafio no cotidiano da equipe de enfermagem. Rev Enferm UFPE on line.2016;10(Supl. 6):4820-7. Available from: https://bit.ly/3OOCi6g
Rodrigues RSM, Reibnitz, KS. Estratégias de captação de doadores de sangue: uma revisão integrativa da literatura. Texto Contexto Enferm. 2011;20(2):384-91. Available from: https://doi.org/10.1590/S0104-07072011000200022 DOI: https://doi.org/10.1590/S0104-07072011000200022
Brasil. Ministério da Saúde. Portaria de Consolidação nº 5, de 28 de setembro de 2017. Consolidação das normas sobre as ações e os serviços de saúde do Sistema Único de Saúde. Diário Oficial da União [Internet]. Brasília, Sep 28, 2017; p. 360. Available from: https://bit.ly/3PQPHvU
Brasil. Presidência da República. Subchefia para Assuntos Jurídicos. Constituição da República Federativa do Brasil de 1988 [Internet]. Brasília, Oct 05, 1998. Available from: https://bit.ly/3QgGM6I
Brasil. Agência Nacional de Vigilância Sanitária. Diretoria Colegiada. Resolução - RDC nº 34, de 11 de junho de 2014. Dispõe sobre as boas práticas no ciclo do sangue. Diário Oficial da União [Internet]. Brasília, Jun 11, 2014. Available from: https://bit.ly/3PX105U
Monteiro LAS, Duarte ACG, Mota GAR, Correa RD, Santos FBO, Almeida SP. Seleção de doador em serviço de hemoterapia: desafios da equipe de assistência ao paciente no processo de triagem clínica. Rev Min Enferm. 2021;25:e-1358. http://doi.org/10.5935/1415.2762.20210006 DOI: https://doi.org/10.5935/1415.2762.20210006
World Health Organization. Toward 100% Voluntary Blood Donation: A Global Framework for Action. World Health Organization. [Internet]. Geneva: WHO; 2010. [cited 18 Jun 2021];11-25. Available from: https://apps.who.int/iris/handle/10665/44359
World Health Organization. Blood safety and availability [Internet]. Geneva: WHO; 2019. [cited 18 Jun 2021]. Available from: https://bit.ly/3vzrYs5
Brasil. Agência Nacional de Vigilância Sanitária. 8º Boletim de Produção Hemoterápica: Produção Hemoterapica no Brasil [Internet]; Brasília, 2021. [cited 18 Jun 2021]. Available from: https://bit.ly/3zutgWi
Souza MKF, Santoro P. Desafios e estratégias para doação de sangue e autossuficiência sob perspectivas regionais da Espanha e do Brasil. Cad Saúde Coletiva. 2019;27(2):195-201. https://doi.org/10.1590/1414-462x201900020068 DOI: https://doi.org/10.1590/1414-462x201900020068
Liberato SMD, Costa IKF, Pessoa CM, Nogueira MAC, Araújo MDMN, Torres GV. Perfil dos doadores de sangue do hemocentro público de Natal/RN. Rev Pesq Cuid Fundam Online. 2013;5(1):3523-30. https://doi.org/10.9789/2175-5361.2013v5n1p3523 DOI: https://doi.org/10.9789/2175-5361.2013.v5i1.3523-3530
Santos AKS, Viana AIS, Menezes ACCL, Marino LB. Perfil dos doadores de sangue inaptos em triagem sorológica em um hemonúcleo no interior do Maranhão. Rev Patologia Tocantins. 2020;7(4):19-25. https://doi.org/10.20873/uft.2446-6492.2020v7n4p19 DOI: https://doi.org/10.20873/uft.2446-6492.2020v7n4p19
Tagny CT, Laperche S, Murphy EL, Francophone Africa Network for Transfusion Medicine Research. Updated characteristics of blood services, donors and blood products in 11 French-speaking African countries. Vox Sang. 2018;113(7):647-656. https://doi.org/10.1111/vox.12702 DOI: https://doi.org/10.1111/vox.12702
Mowla SJ, Sapiano M, Jones JM, Berger JJ, Basavaraju SV. Supplemental findings of the 2019 National Blood Collection and Utilization Survey. Transfusion. 2021;61 Suppl 2(Suppl 2):11-35. https://doi.org/10.1111/trf.16606 DOI: https://doi.org/10.1111/trf.16606
Bezerra AGN, Leal VS, Lira PIC, Oliveira JS, Costa EC, Menezes RCE, et al. Anemia e fatores associados em mulheres de idade reprodutiva de um município do Nordeste brasileiro. Rev Bras Epidemiol. 2018;21:e180001. https://doi.org/10.1590/1980-549720180001 DOI: https://doi.org/10.1590/1980-549720180001
Melo MC, Cristo RC, Guilhem D. Perfil sociodemográfico de acompanhantes de pacientes e suas concepções sobre atenção recebida. Rev Gestão Saúde. 2015;6(2):1550-64. https://doi.org/10.18673/gs.v6i2.22485 DOI: https://doi.org/10.18673/gs.v6i2.22485
Shash H, Alabdulqader R, Alshehri L, Alkathery N, Al-Abdulrahman R, Alahmed S, et al. Blood utilization and quality indicators at a university hospital in the Eastern Province of Saudi Arabia. PLoS ONE. 2022;17(4): e0267449. https://doi.org/10.1371/journal.pone.0267449 DOI: https://doi.org/10.1371/journal.pone.0267449
Haddad A, Bou Assi T, Baz E, Samaha H, Hachem B, Feghali R, Jisr T et al. Blood donations mode: Assessment of the Lebanese model. Transfus Clin Biol. 2019;26(4):341-5. https://doi.org/10.1016/j.tracli.2019.02.009 DOI: https://doi.org/10.1016/j.tracli.2019.02.009
Auvinen MK, Zhao J, Lassén E, et al. Patterns of blood use in Sweden from 2008 to 2017: A nationwide cohort study. Transfusion. 2020;60(11):2529-36. https://doi.org/10.1111/trf.16092 DOI: https://doi.org/10.1111/trf.16092
Bou Assi T, Haddad A, Haddad L, Garraud O. Can a decentralized blood supply system reach 100% voluntary nonremunerated donation?. Int J Health Plann Manage. 2018;33(4):e883-91. https://doi.org/10.1002/hpm.2576 DOI: https://doi.org/10.1002/hpm.2576
Hirani R, Weinert N, Irving DO. The distribution of ABO RhD blood groups in Australia, based on blood donor and blood sample pathology data. Med J Aust. 2022;216(6):291-5. https://doi.org/10.5694/mja2.51429 DOI: https://doi.org/10.5694/mja2.51429
Rohr JI, Boff D, Lunkes DS. Perfil dos candidatos inaptos para doação de sangue no serviço de hemoterapia do hospital Santo Ângelo, RS, Brasil. Rev Patol Trop. 2012;41(1):23-35. https://doi.org/10.5216/rpt.v41i1.17750 DOI: https://doi.org/10.5216/rpt.v41i1.17750
Kim HO. Current state of blood management services in Korea. Ann Lab Med. 2022;42:306-13. https://doi.org/10.3343/alm.2022.42.3.306 DOI: https://doi.org/10.3343/alm.2022.42.3.306
Cicolini G, Comparcini, D, Alfieri S, Zito E, Marta E, Tomietto M, et al. Nursing students' knowledge and attitudes of blood donation: A multicentre study. J Clin Nursing. 2019;28(9-10):1829-38. https://doi.org/10.1111/jocn.14792 DOI: https://doi.org/10.1111/jocn.14792
Valerian DM, Mauka WI, Kajeguka DC, Mgabo M, Juma A, Baliyima L, et al. Prevalence and causes of blood donor deferrals among clients presenting for blood donation in northern Tanzania. PLoS ONE. 2018; 13(10): e0206487. https://doi.org/10.1371/journal.pone.0206487 DOI: https://doi.org/10.1371/journal.pone.0206487
Costa LSL, Eleuterio TA, Pereira SS, Santiago SC, Bandeira, Flavia MGC. Perfil epidemiológico do doador voluntário de sangue em um Hospital Universitário no Rio de Janeiro. Rev Saúde (Santa Maria).2020;46(2):e43186. https://doi.org/10.5902/2236583443186 DOI: https://doi.org/10.5902/2236583443186
Carlesso L, Guimarães RFS, Silva SL, Santos CF, Viero V, Vieira SV. Estratégias implementadas em hemocentros para aumento da doação de sangue. Rev Bras Prom Saúde. 2017;30(2):213-20. https://doi.org/10.5020/18061230.2017.p213 DOI: https://doi.org/10.5020/18061230.2017.p213
Silva, JR, Brasil CCP, Filho JEV, Brasil BP, Paiva LB, Oliveira VF. Aplicativo de apoio à doação de sangue: contribuições de especialistas sobre a funcionalidade da ferramenta. Ciênc Saúde Coletiva. 2021;26(2):493-503. https://doi.org/10.1590/1413-81232021262.41022020 DOI: https://doi.org/10.1590/1413-81232021262.41022020
Bruhin A, Goette L, Haenni S, Jiang L. Spillovers of prosocial motivation: evidence from an intervention study on blood donors. J Health Econom. 2020;70:102244. https://doi.org/10.1016/j.jhealeco.2019.102244 DOI: https://doi.org/10.1016/j.jhealeco.2019.102244