Effects of omega-3 supplementation associated with physical activity in obese patients with type 2 diabetes mellitus: study protocol
Main Article Content
Abstract
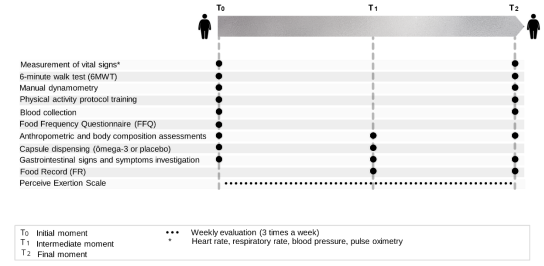
Objective: This study aims to evaluate the effects of omega-3-rich fish oil supplementation with or without physical activity on anti-inflammatory and insulin resistance parameters in obese and type 2 diabetic individuals. Methods: Randomized, double-blind intervention study of omega-3. Adults with obesity and type 2 diabetes mellitus on exclusive use of metformin as a drug to control blood glucose will be included. The Protocol will be based on clinical and nutritional follow-up (supplementation with omega-3) and remote physical activity for eight weeks. Individuals selected for the study will be randomly assigned to one of the following groups: i) omega-3; ii) omega-3 + physical activity; iii) physical activity + placebo; iv) placebo. To analyze the results, biochemical parameters (fasting glucose and insulin, glycosylated hemoglobin, liver enzymes, urea, creatinine, total cholesterol and fractions, triglycerides, CRP, and ferritin) and inflammatory parameters (TNF alpha, IL-1 beta, IL- 6 and IL-10). At the end of the study, it is expected that the intervention associated with omega-3 in the physical activity protocol will promote a reduction in parameters related to insulin resistance, levels of inflammatory cytokines, and anthropometric parameters.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
McCracken E, Monaghan M, Sreenivasan S. Pathophysiology of the metabolic syndrome. Clin Dermatol. 2018;36(1):14-20. https://doi.org/10.1016/j.clindermatol.2017.09.004
Brasil, Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise em Saúde e Vigilância de Doenças não Transmissíveis. VIGITEL BRASIL 2018: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico Estimativas Sobre Frequência e Distribuição Sociodemográfica de Fatores de Risco e Proteção para Doenças Crônicas nas Capitais dos 26 Estados Brasileiros e no Distrito Federal em 2018. Brasilia, DF: Ministério da Saúde; 2019. 132 p. http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2018_vigilancia_fatores_risco.pdf
Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20(2):1-8. https://doi.org/10.1007/s11906-018-0812-z
Roden M, Shulman GI. The integrative biology of type 2 diabetes. Nature. 2019;576(7785):51-60. https://doi.org/10.1038/s41586-019-1797-8
Souza CT. Envolvimento da inflamação subclínica e do estresse oxidativo na resistência à insulina associada a obesidade. HU Revista. 2018;44(2):211-20. https://doi.org/10.34019/1982-8047.2018.v44.16950
Lois K, Valsamakis G, Mastorakos G, Kumar S. The impact of insulin resistance on woman's health and potential treatment options. Ann N Y Acad Sci. 2010;1205(1):156-65. https://doi.org/10.1111/j.1749-6632.2010.05646.x
Pahlavani M, Ramalho T, Koboziev I, LeMieux MJ, Jayarathne S, Ramalingam L, et al. Adipose tissue inflammation in insulin resistance: review of mechanisms mediating anti-inflammatory effects of omega-3 polyunsaturated fatty acids. J Investig Med. 2017;65(7):1021-7. https://doi.org/10.1136/jim-2017-000535
Cintra DE, Ropelle ER, Silva ASR, Souza CT, Pauli JR. Sinalização celular e exercício físico. In: Cintra DE, Ropelle ER, Pauli JR, editors. Obesidade e Diabetes: Fisiopatologia e Sinalização Celular. 1 ed. São Paulo: Sarvier; 2011. p. 74-99.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377-81. https://pubmed.ncbi.nlm.nih.gov/7154893/
Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. Questionário Internacional de Atividade Física (IPAQ): Estudo de Validade e Reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2012;6(2):5-18. https://doi.org/10.12820/rbafs.v.6n2p5-18
WHO Expert Committee on Physical Status, World Health Organization. Physical status: the use of and interpretation of anthropometry , report of a WHO expert committee. Geneva, Switzerland: World Health Organization; 1995. 854 p. https://apps.who.int/iris/handle/10665/37003
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7. https://doi.org/10.1164/ajrccm.166.1.at1102
American College of Sports Medicine (ACSM's). ACSM's Guidelines for Exercise Testing and Prescription 9ed. Philadelphia: Lippincott Williams & Wilkins; 2014. 546 p.
Klika B, Jordan C. High-intensity circuit training using body weight: Maximum results with minimal investment. ACSMs Health Fit J. 2013;17(3):8-13. http://doi.org/10.1249/FIT.0b013e31828cb1e8
Souza DR, Pieri BLS, Comim VH, Marques SO, Luciano TF, Rodrigues MS, et al. Fish oil reduces subclinical inflammation, insulin resistance, and atherogenic factors in overweight/obese type 2 diabetes mellitus patients: A pre-post pilot study. J Diabetes Complications. 2020;34(5):107553. https://doi.org/10.1016/j.jdiacomp.2020.107553