Characteristics and effects of physical exercise programs for older adults during the COVID-19 pandemic: an integrative review
Main Article Content
Abstract
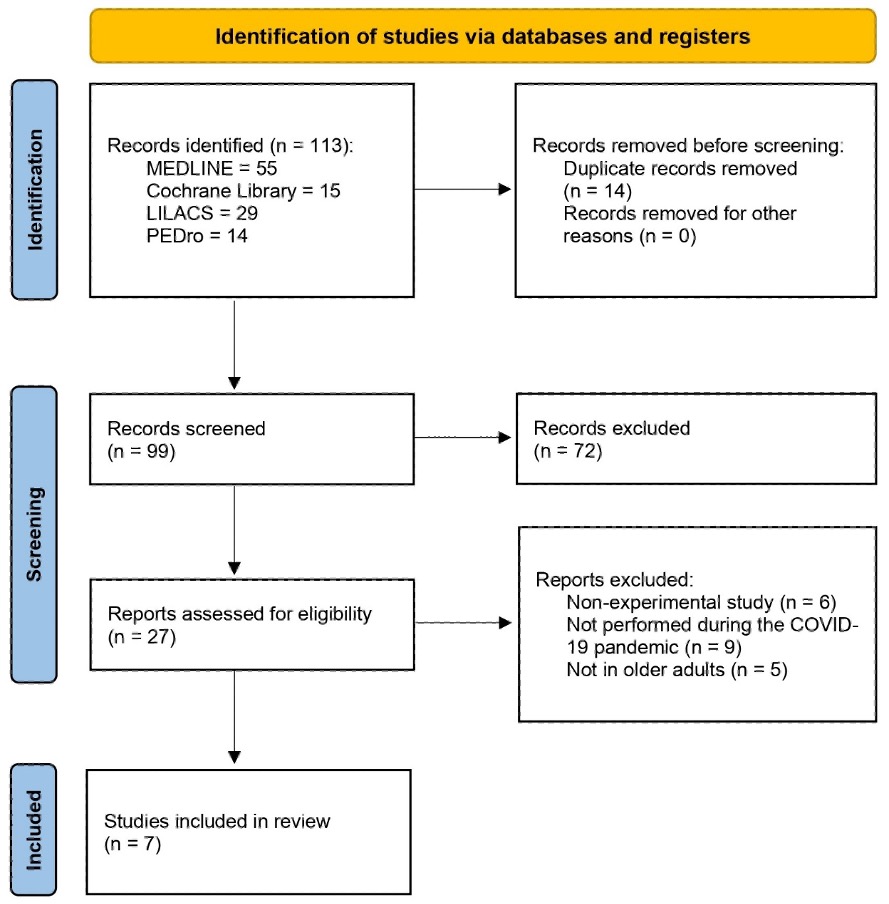
Objective: To evaluate the characteristics of physical exercise programs for older adults and their effects during the COVID-19 pandemic. Methods: An integrative review was conducted between January and March 2022. A search was conducted in MEDLINE via PubMed, Lilacs via BVS, PEDro, and Cochrane Library. Experimental articles (randomized clinical trials, non-randomized trials, or quasi-experimental studies) published from 2019 to 2021, with no language restriction, and that used physical exercise programs for older adults (> 60 years) in their intervention were included. The studies were selected by reading the title, abstract, and full text. The selected articles had their results extracted using an online form, tabulated using an electronic spreadsheet, and analyzed qualitatively and quantitatively. Results: 113 studies were identified; 7 met the eligibility criteria and were included in the review, all randomized controlled trials. The multi-component exercise programs were more frequent (resistance, balance, flexibility, and aerobic), delivered remotely and performed 2 to 7 times a week, lasting between 30 and 50 minutes. Significant effects were observed on physical function, body composition, blood triglycerides, the incidence of falls, physical activity, and functional capacity. Conclusions: The physical exercise programs used during the COVID-19 pandemic showed promising results for older adults. The programs proved to be a viable alternative for maintaining the physical, mental, and cognitive functions of older adults in times of public calamity.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-60. https://doi.org/10.23750/abm.v91i1.9397
Richardson DL, Duncan MJ, Clarke ND, Myers TD, Tallis J. The influence of COVID-19 measures in the United Kingdom on physical activity levels, perceived physical function and mood in older adults: A survey-based observational study. J Sports Sci. 2021;39(8):887-99. https://doi.org/10.1080/02640414.2020.1850984 DOI: https://doi.org/10.1080/02640414.2020.1850984
Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Heal Res Policy. 2020;5(1):27. https://doi.org/10.1186/s41256-020-00154-3 DOI: https://doi.org/10.1186/s41256-020-00154-3
Bezerra GKSD, Sousa ACPA, Araújo MCM, Lucena GA, Fernandes LFQ, Morais PHM, et al. Efeitos do isolamento social para a saúde de pessoas idosas no contexto da pandemia de Covid-19: um estudo de revisão integrativa. Res Soc Dev. 2021;10(4):e23010414070. https://doi.org/10.33448/rsd-v10i4.14070 DOI: https://doi.org/10.33448/rsd-v10i4.14070
Kucharski AJ, Klepac P, Conlan AJK, Kissler SM, Tang ML, Fry H, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20(10):1151-60. https://doi.org/10.1016/S1473-3099(20)30457-6 DOI: https://doi.org/10.1016/S1473-3099(20)30457-6
Qin F, Song Y, Nassis GP, Zhao L, Dong Y, Zhao C, et al. Physical Activity, Screen Time, and Emotional Well-Being during the 2019 Novel Coronavirus Outbreak in China. Int J Environ Res Public Health. 2020;17(14):5170. https://doi.org/10.3390/ijerph17145170 DOI: https://doi.org/10.3390/ijerph17145170
Schuch FB, Bulzing RA, Meyer J, Vancampfort D, Firth J, Stubbs B, et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: A cross-sectional survey in Brazil. Psychiatry Res. 2020;292:113339. https://doi.org/10.1016/j.psychres.2020.113339 DOI: https://doi.org/10.1016/j.psychres.2020.113339
Roschel H, Artioli GG, Gualano B. Risk of Increased Physical Inactivity During COVID‐19 Outbreak in Older People: A Call for Actions. J Am Geriatr Soc. 2020;68(6):1126-8. https://doi.org/10.1111/jgs.16550 DOI: https://doi.org/10.1111/jgs.16550
Brasil, Ministério da Saúde. Pesquisa nacional de saúde: 2019: percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal: Brasil e grandes regiões. IBGE (ed). Rio de Janeiro; 2020 [cited 2023 Mar 19]. 105 p. Available from: https://bit.ly/3TH7LeV
Silva DRP, Werneck AO, Malta DC, Souza Júnior PRB, Azevedo LO, Barros MBA, et al. Changes in the prevalence of physical inactivity and sedentary behavior during COVID-19 pandemic: a survey with 39,693 Brazilian adults. Cad Saude Publica. 2021;37(3):e00221920. https://doi.org/10.1590/0102-311x00221920 DOI: https://doi.org/10.1590/0102-311x00221920
Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz Martínez BJ, et al. Post-COVID-19 Syndrome and the Potential Benefits of Exercise. Int J Environ Res Public Health. 2021;18(10):5329. https://doi.org/10.3390/ijerph18105329 DOI: https://doi.org/10.3390/ijerph18105329
Silva Filho E, Xavier J, Cezarino L, Sales H, Albuquerque J. Comment on "The importance of physical exercise during the coronavirus (COVID-19) pandemic." Rev Assoc Med Bras. 2020;66(9):1311-3. https://doi.org/10.1590/1806-9282.66.9.1311 DOI: https://doi.org/10.1590/1806-9282.66.9.1311
Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Context - Enferm. 2008;17(4):758-64. https://doi.org/10.1590/S0104-07072008000400018 DOI: https://doi.org/10.1590/S0104-07072008000400018
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-73. https://doi.org/10.7326/M18-0850 DOI: https://doi.org/10.7326/M18-0850
Santos CMC, Pimenta CAM, Nobre MRC. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15(3):508-11. https://doi.org/10.1590/S0104-11692007000300023 DOI: https://doi.org/10.1590/S0104-11692007000300023
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4 DOI: https://doi.org/10.1186/s13643-016-0384-4
Grant D, Tomlinson D, Tsintzas K, Kolić P, Onambele-Pearson GL. The Effects of Displacing Sedentary Behavior With Two Distinct Patterns of Light Activity on Health Outcomes in Older Adults (Implications for COVID-19 Quarantine). Front Physiol. 2020;11:574595. https://doi.org/10.3389/fphys.2020.574595 DOI: https://doi.org/10.3389/fphys.2020.574595
Vitale JA, Bonato M, Borghi S, Messina C, Albano D, Corbetta S, et al. Home-Based Resistance Training for Older Subjects during the COVID-19 Outbreak in Italy: Preliminary Results of a Six-Months RCT. Int J Environ Res Public Health. 2020;17(24):9533. https://doi.org/10.3390/ijerph17249533 DOI: https://doi.org/10.3390/ijerph17249533
Beauchamp MR, Hulteen RM, Ruissen GR, Liu Y, Rhodes RE, Wierts CM, et al. Online-Delivered Group and Personal Exercise Programs to Support Low Active Older Adults' Mental Health During the COVID-19 Pandemic: Randomized Controlled Trial. J Med Internet Res. 2021;23(7):e30709. https://doi.org/10.2196/30709 DOI: https://doi.org/10.2196/30709
Li F, Harmer P, Voit J, Chou L-S. Implementing an Online Virtual Falls Prevention Intervention During a Public Health Pandemic for Older Adults with Mild Cognitive Impairment: A Feasibility Trial. Clin Interv Aging. 2021;16:973-83. https://doi.org/10.2147/CIA.S306431 DOI: https://doi.org/10.2147/CIA.S306431
Liang IJ, Perkin OJ, McGuigan PM, Thompson D, Western MJ. Feasibility and Acceptability of Home-Based Exercise Snacking and Tai Chi Snacking Delivered Remotely to Self-Isolating Older Adults During COVID-19. J Aging Phys Act. 2022;30(1):33-43. https://doi.org/10.1123/japa.2020-0391 DOI: https://doi.org/10.1123/japa.2020-0391
Chen X, Zhao L, Liu Y, Zhou Z, Zhang H, Wei D, et al. Otago exercise programme for physical function and mental health among older adults with cognitive frailty during COVID‐19: A randomised controlled trial. J Clin Nurs. 2021;10.1111/locn.15964. https://doi.org/10.1111/jocn.15964 DOI: https://doi.org/10.1111/jocn.15964
Courel-Ibáñez J, Pallarés JG, García-Conesa S, Buendía-Romero Á, Martínez-Cava A, Izquierdo M. Supervised Exercise (Vivifrail) Protects Institutionalized Older Adults Against Severe Functional Decline After 14 Weeks of COVID Confinement. J Am Med Dir Assoc . 2021;22(1):217-219.e2. https://doi.org/10.1016/j.jamda.2020.11.007 DOI: https://doi.org/10.1016/j.jamda.2020.11.007
Lee K, Jeong G-C, Yim J. Consideration of the Psychological and Mental Health of the Elderly during COVID-19: A Theoretical Review. Int J Environ Res Public Health. 2020;17(21):8098. https://doi.org/10.3390/ijerph17218098 DOI: https://doi.org/10.3390/ijerph17218098
Baez M, Khaghani Far I, Ibarra F, Ferron M, Didino D, Casati F. Effects of online group exercises for older adults on physical, psychological and social wellbeing: a randomized pilot trial. Peer J. 2017;5:e3150. https://doi.org/10.7717/peerj.3150 DOI: https://doi.org/10.7717/peerj.3150
Yerrakalva D, Yerrakalva D, Hajna S, Griffin S. Effects of Mobile Health App Interventions on Sedentary Time, Physical Activity, and Fitness in Older Adults: Systematic Review and Meta-Analysis. J Med Internet Res. 2019;21(11):e14343. https://doi.org/10.2196/14343 DOI: https://doi.org/10.2196/14343
Guimarães JAC, Guerra PH, Ueno DT, Christofoletti AEM, Nakamura PM. Estudo transversal sobre uso de ferramentas virtuais para orientar a atividade física durante a COVID-19. Rev Bras Ativ Fís Saúde. 2020;25:1-8. https://doi.org/10.12820/rbafs.25e0150 DOI: https://doi.org/10.12820/rbafs.25e0150
World Health Organization. COVID-19 transmission and protective measures [Internet]. 2022 [updated 21 Sep 2022]. Available from: http://bit.ly/3lvcKlV
Centers for Disease Control and Prevention. COVID-19 Risks and Inormation for Older Adults [Internet]. [updated 22 Feb 2023]. Available from: http://bit.ly/3n2rrgO
Pradhan D, Biswasroy P, Kumar Naik P, Ghosh G, Rath G. A Review of Current Interventions for COVID-19 Prevention. Arch Med Res. 2020;51(5):363-74. https://doi.org/10.1016/j.arcmed.2020.04.020 DOI: https://doi.org/10.1016/j.arcmed.2020.04.020
Lima Junior LC. Alimentação saudável e exercícios físicos em meio à pandemia da Covid-19. Bol Conjunt. 2020;3(9):33-41. Available from: https://bit.ly/3JR8ZAU
Santos DAS, Fernandes CC, Watanabe LAR. Cinesioterapia em Idosos de Instituições de Longa Permanência. Amaz Sci Heal. 2016;4(4):32-6. Available from: https://bit.ly/3yP2ZlH DOI: https://doi.org/10.18606/2318-1419/amazonia.sci.health.v4n4p32-36
Rugbeer N, Ramklass S, Mckune A, van Heerden J. The effect of group exercise frequency on health related quality of life in institutionalized elderly. Pan Afr Med J. 2017;26:35. https://doi.org/10.11604/pamj.2017.26.35.10518 DOI: https://doi.org/10.11604/pamj.2017.26.35.10518
Espejo-Antúnez L, Pérez-Mármol JM, Cardero-Durán MÁ, Toledo-Marhuenda JV, Albornoz-Cabello M. The Effect of Proprioceptive Exercises on Balance and Physical Function in Institutionalized Older Adults: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2020;101(10):1780-8. https://doi.org/10.1016/j.apmr.2020.06.010 DOI: https://doi.org/10.1016/j.apmr.2020.06.010
Borges-Machado F, Silva N, Farinatti P, Poton R, Ribeiro Ó, Carvalho J. Effectiveness of Multicomponent Exercise Interventions in Older Adults With Dementia: A Meta-Analysis. Gerontologist. 2021;61(8):e449-62. https://doi.org/10.1093/geront/gnaa091 DOI: https://doi.org/10.1093/geront/gnaa091
Sadjapong U, Yodkeeree S, Sungkarat S, Siviroj P. Multicomponent Exercise Program Reduces Frailty and Inflammatory Biomarkers and Improves Physical Performance in Community-Dwelling Older Adults: A Randomized Controlled Trial. Int J Environ Res Public Health. 2020;17(11):3760. https://doi.org/10.3390/ijerph17113760 DOI: https://doi.org/10.3390/ijerph17113760
Roy J, Jain R, Golamari R, Vunnam R, Sahu N. COVID‐19 in the geriatric population. Int J Geriatr Psychiatry. 2020;35(12):1437-41. https://doi.org/10.1002/gps.5389 DOI: https://doi.org/10.1002/gps.5389
Cadore EL, Sáez de Asteasu ML, Izquierdo M. Multicomponent exercise and the hallmarks of frailty: Considerations on cognitive impairment and acute hospitalization. Exp Gerontol. 2019;122:10-4https://doi.org/10.1016/j.exger.2019.04.007 DOI: https://doi.org/10.1016/j.exger.2019.04.007
Freiberger E, Häberle L, Spirduso WW, Rixt Zijlstra GA. Long‐Term Effects of Three Multicomponent Exercise Interventions on Physical Performance and Fall‐Related Psychological Outcomes in Community‐Dwelling Older Adults: A Randomized Controlled Trial. J Am Geriatr Soc. 2012;60(3):437-46. https://doi.org/10.1111/j.1532-5415.2011.03859.x DOI: https://doi.org/10.1111/j.1532-5415.2011.03859.x
Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J Nutr Health Aging. 2021;25(7):824-53. https://doi.org/10.1007/s12603-021-1665-8 DOI: https://doi.org/10.1007/s12603-021-1665-8
World Health Organization. Guidelines on physical activity and sedentary behaviour: at a glance. World Health Organization: Geneva; 25 Nov 2020 [cited 19 Mar 2023]. Available from: http://bit.ly/3LyoPS4
Lazarus NR, Izquierdo M, Higginson IJ, Harridge SDR. Exercise Deficiency Diseases of Ageing: The Primacy of Exercise and Muscle Strengthening as First-Line Therapeutic Agents to Combat Frailty. J Am Med Dir Assoc. 2018;19(9):741-3. https://doi.org/10.1016/j.jamda.2018.04.014 DOI: https://doi.org/10.1016/j.jamda.2018.04.014
Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1-72. https://doi.org/10.1111/sms.12581 DOI: https://doi.org/10.1111/sms.12581
Zhao M, Veeranki SP, Magnussen CG, Xi B. Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study. BMJ. 2020;370:m2031. https://doi.org/10.1136/bmj.m2031 DOI: https://doi.org/10.1136/bmj.m2031
Wade KH, Richmond RC, Davey Smith G. Physical activity and longevity: how to move closer to causal inference. Br J Sports Med. 2018;52(14):890-1. https://doi.org/10.1136/bjsports-2017-098995 DOI: https://doi.org/10.1136/bjsports-2017-098995
Stensvold D, Viken H, Steinshamn SL, Dalen H, Støylen A, Loennechen JP, et al. Effect of exercise training for five years on all-cause mortality in older adults-the Generation 100 study: randomised controlled trial. BMJ. 2020;m3485. https://doi.org/10.1136/bmj.m3485 DOI: https://doi.org/10.1136/bmj.m3485
Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog Cardiovasc Dis. 2020;63(3):386-8. https://doi.org/10.1016/j.pcad.2020.03.009 DOI: https://doi.org/10.1016/j.pcad.2020.03.009
Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, Ganz F, Torralba R, Oliveira D V, et al. Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J Nutr Health Aging. 2020;24(9):938-47. https://doi.org/10.1007/s12603-020-1469-2 DOI: https://doi.org/10.1007/s12603-020-1500-7
Dipietro L, Campbell WW, Buchner DM, Erickson KI, Powell KE, Bloodgood B, et al. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med Sci Sport Exerc. 2019;51(6):1303-13. https://doi.org/10.1249/MSS.0000000000001942 DOI: https://doi.org/10.1249/MSS.0000000000001942
Theodorakopoulos C, Jones J, Bannerman E, Greig CA. Effectiveness of nutritional and exercise interventions to improve body composition and muscle strength or function in sarcopenic obese older adults: A systematic review. Nutr Res. 2017;43:3-15. https://doi.org/10.1016/j.nutres.2017.05.002 DOI: https://doi.org/10.1016/j.nutres.2017.05.002
Chen N, He X, Feng Y, Ainsworth BE, Liu Y. Effects of resistance training in healthy older people with sarcopenia: a systematic review and meta-analysis of randomized controlled trials. Eur Rev Aging Phys Act. 2021;18(1):23. https://doi.org/10.1186/s11556-021-00277-7 DOI: https://doi.org/10.1186/s11556-021-00277-7
Blasco-Lafarga C, Monteagudo P, Roldán A, Cordellat A, Pesce C. Strategies to change body composition in older adults: do type of exercise and dose distribution matter? J Sports Med Phys Fitness. 2020;60(4):552-61. https://doi.org/10.23736/S0022-4707.20.10321-9 DOI: https://doi.org/10.23736/S0022-4707.20.10321-9
da Rosa Orssatto LB, de la Rocha Freitas C, Shield AJ, Silveira Pinto R, Trajano GS. Effects of resistance training concentric velocity on older adults' functional capacity: A systematic review and meta-analysis of randomised trials. Exp Gerontol. 2019;127:110731. https://doi.org/10.1016/j.exger.2019.110731 DOI: https://doi.org/10.1016/j.exger.2019.110731
Liu C, Shiroy DM, Jones LY, Clark DO. Systematic review of functional training on muscle strength, physical functioning, and activities of daily living in older adults. Eur Rev Aging Phys Act. 2014;11(2):95-106. https://doi.org/10.1007/s11556-014-0144-1 DOI: https://doi.org/10.1007/s11556-014-0144-1
Telenius EW, Engedal K, Bergland A. Long-term effects of a 12 weeks high-intensity functional exercise program on physical function and mental health in nursing home residents with dementia: a single blinded randomized controlled trial. BMC Geriatr. 2015;15(1):158. https://doi.org/10.1186/s12877-015-0151-8 DOI: https://doi.org/10.1186/s12877-015-0151-8
Raafs BM, Karssemeijer EGA, Van der Horst L, Aaronson JA, Olde Rikkert MGM, Kessels RPC. Physical Exercise Training Improves Quality of Life in Healthy Older Adults: A Meta-Analysis. J Aging Phys Act. 2020;28(1):81-93. https://doi.org/10.1123/japa.2018-0436 DOI: https://doi.org/10.1123/japa.2018-0436
Paluska SA, Schwenk TL. Physical Activity and Mental Health. Sport Med. 2000;29(3):167-80. https://doi.org/10.2165/00007256-200029030-00003 DOI: https://doi.org/10.2165/00007256-200029030-00003