Stress levels and related factors in primary care health professionals: an integrative review
Main Article Content
Abstract
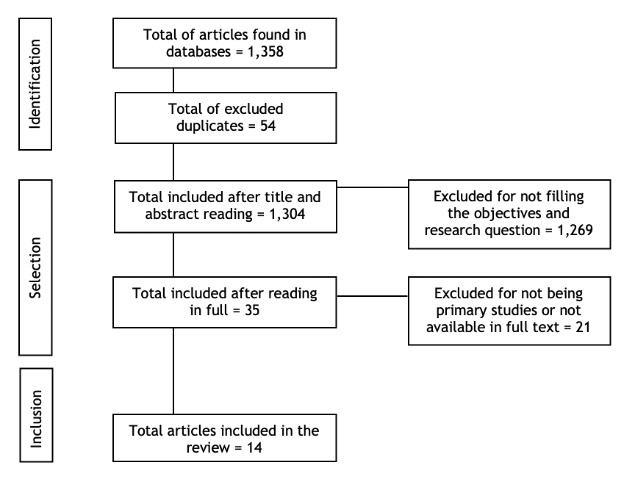
Objective: To identify, based on evidence, stress levels and related factors in health professionals working in Primary Care. Methods: An integrative review was carried out, with the guiding question "What are the levels of stress and factors related to them in health professionals working in Primary Care?". The research took place in December 2022, in the databases: LILACS, MEDLINE, CINAHL and Scopus. Primary studies available in full in English, Portuguese and Spanish were included. Results: Of the 1,358 productions initially found, 14 texts were included as a sample. It was observed that professionals face different levels of stress in their daily
work. Stress can be related to physical and emotional exhaustion, dissatisfaction, overload and less engagement at work, longer working hours, female sex, work in the Covid-19 pandemic, organizational and communication problems. Conclusions: The evidence allows critical reflection on the need for greater concern and involvement on the part of the authorities and competent bodies with the health of workers, in order to direct actions that can intervene on risk factors in the work environment and minimize vulnerabilities caused by stress.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Pascoal FFS, Evangelista CB, Pascoal KPMF, Batista JBV, Rodrigues MSD, Souza GP. Síndrome de burnout: conhecimento da equipe saúde do trabalhador. Rev Pesq Cuid Fundam Online. 2021;13:302-8. https://doi.org/10.9789/2175-5361.rpcfo.v13.8567 DOI: https://doi.org/10.9789/2175-5361.rpcfo.v13.8567
Munhoz OL, Arrial TS, Barlem ELD, Dalmolin GL, Andolhe R, Magnago TSBS. Estresse ocupacional e burnout em profissionais de saúde de unidades de perioperatório. Acta Paul Enferm. 2020;33:eAPE20190261. https://doi.org/10.37689/acta-ape/2020AO0261 DOI: https://doi.org/10.37689/acta-ape/2020AO0261
Fernandes LS, Nitsche MJT, Godoy ID. Síndrome de burnout em profissionais de enfermagem de uma unidade de terapia intensiva. Rev Pesq Cuid Fundam Online. 2017;9(2):551-7. https://doi.org/10.9789/2175-5361.2017.v9i2.551-557 DOI: https://doi.org/10.9789/2175-5361.2017.v9i2.551-557
Carvalho AEL, Frazão IS, Silva DMR, Andrade MS, Vasconcelos SC, Aquino JM. Stress of nursing professionals working in pre-hospital care. Rev Bras Enferm. 2020;73(2):e20180660. https://doi.org/10.1590/0034-7167-2018-0660 DOI: https://doi.org/10.1590/0034-7167-2018-0660
Esteves GGL, Leão AAM, Alves EO. Fadiga e Estresse como preditores do Burnout em Profissionais da Saúde. Rev Psicol Org Trab. 2019;19(3):695-702. https://doi.org/10.17652/rpot/2019.3.16943 DOI: https://doi.org/10.17652/rpot/2019.3.16943
Ribeiro KV, Peixoto EM, Velasque LS, Vieira GC, Oliveira EB, Passos JP. Estresse ocupacional e fatores estressores em enfermeiros de unidades de internação clínica. Rev Baiana Saúde Pública. 2020;44(2):81-94. https://doi.org/10.22278/2318-2660.2020.v44.n2.a3110 DOI: https://doi.org/10.22278/2318-2660.2020.v44.n2.a3110
Sousa MF, Santos BMP, Paz EPA, Alvarenga JDPO. Complexidade das Práticas da Enfermagem na Atenção Primária à Saúde. Enferm Foco. 2021;12(Supl.1):55-60. https://doi.org/10.21675/2357-707X.2021.v12.n7.SUPL.1.5211 DOI: https://doi.org/10.21675/2357-707X.2021.v12.n7.SUPL.1.5211
Lima GKM, Gomes LMX, Barbosa TLA. Qualidade de Vida no Trabalho e nível de estresse dos profissionais da atenção primária. Saúde Debate. 2020;44(126):774-89. https://doi.org/10.1590/0103-1104202012614 DOI: https://doi.org/10.1590/0103-1104202012614
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546-53. https://doi.org/10.1111/j.1365-2648.2005.03621.x DOI: https://doi.org/10.1111/j.1365-2648.2005.03621.x
Souza MT, Silva MD, Carvalho R. Integrative review: what is it? How to do it? Einstein (São Paulo). 2010;8(1):102-6. https://doi.org/10.1590/s1679-45082010rw1134 DOI: https://doi.org/10.1590/s1679-45082010rw1134
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Systematic Reviews. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4 DOI: https://doi.org/10.1186/s13643-016-0384-4
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372(71):n71. https://doi.org/10.1136/bmj.n71 DOI: https://doi.org/10.1136/bmj.n71
Garcia GPA, Marziale MHP. Satisfaction, stress and burnout of nurse managers and care nurses in Primary Health Care. Rev Escola Enferm USP. 2021;55:e03675. https://doi.org/10.1590/s1980-220x2019021503675
Stanetić K, Petrović V, Marković B, Stanetić B. The Presence of Stress, Burnout Syndrome and the Most Important Causes of Working Stress Among Physicians in Primary Health Care - an Observational Study from Banja Luka, Bosnia and Herzegovina. Acta Med Acad. 2019;48(2):159. https://doi.org/10.5644/ama2006-124.254 DOI: https://doi.org/10.5644/ama2006-124.254
Lee JK. Job stress, coping and health perceptions of Hong Kong primary care nurses. Int J Nurs Pract. 2003;9(2):86-91. https://doi.org/10.1046/j.1322-7114.2003.00413.x DOI: https://doi.org/10.1046/j.1322-7114.2003.00413.x
Leonelli LB, Andreoni S, Martins P, Kozasa EH, Salvo VL, Sopezki D, et al. Estresse percebido em profissionais da Estratégia Saúde da Família. Rev Bras Epidemiol. 2017;20:286-98. https://doi.org/10.1590/1980-5497201700020009 DOI: https://doi.org/10.1590/1980-5497201700020009
Silva MG, Barros BP. Percepção de Estresse de Servidores na Atenção Básica de Saúde de Dourados-MS. Saúde Redes. 2015;1(04):35-52. https://doi.org/10.18310/2446-4813.2015v1n4p35-52 DOI: https://doi.org/10.18310/2446-4813.2015v1n4p35-52
Guo H, Ni C, Liu C, Li J, Liu S. Perceived job stress among community nurses: A multi-center cross-sectional study. Int J Nurs Pract. 2018;25(1):e12703. https://doi.org/10.1111/ijn.12703 DOI: https://doi.org/10.1111/ijn.12703
Pérez-Guzmán ID, Zonana-Nacach A, Valles-Medina AM. Niveles de estrés en trabajadores de la salud adscritos a unidades de medicina familiar. Rev Med Inst Mex Seguro Soc. 2009;47(5):575-9. Available from: https://www.redalyc.org/articulo.oa?id=457745516018
Brigola S, Tadei Flores M, Bordin D, Martins AS, Adas Saliba Moimaz S, Berger Fadel C. Trabalho do Cirurgião-Dentista no Serviço Público de Saúde e Implicações Sobre o Estresse. Rev APS. 2019;21(3):428-36. https://doi.org/10.34019/1809-8363.2018.v21.16386 DOI: https://doi.org/10.34019/1809-8363.2018.v21.16386
Lee ES, Tan SY, Lee PSS, Koh HL, Soon SWW, Sim K, et al. Perceived stress and associated factors among healthcare workers in a primary healthcare setting: the Psychological Readiness and Occupational Training Enhancement during COVID-19 Time (PROTECT) study. Singapore Med J. 2022;63(1):20-7. https://doi.org/10.11622/smedj.2020163 DOI: https://doi.org/10.11622/smedj.2020163
Lourenção LG, Sodré PC, Gazetta CE, Silva AG, Castro JR, Maniglia JV. Occupational stress and work engagement among primary healthcare physicians: a cross-sectional study. Sao Paulo Med J. 2022;140(6):747-54. https://doi.org/10.1590/1516-3180.2021.0644.r1.10012022 DOI: https://doi.org/10.1590/1516-3180.2021.0644.r1.10012022
Siegrist J, Shackelton R, Link C, Marceau L, von dem Knesebeck O, McKinlay J. Work stress of primary care physicians in the US, UK and German health care systems. Social Sci Med. 2010;71(2):298-304. https://doi.org/10.1016/j.socscimed.2010.03.043 DOI: https://doi.org/10.1016/j.socscimed.2010.03.043
Trifunovic N, Jatic Z, Kulenovic AD. Identification of Causes of the Occupational Stress for Health Providers at Different Levels of Health Care. Med Arch. 2017;71(3):169-72. https://doi.org/10.5455/medarh.2017.71.169-172 DOI: https://doi.org/10.5455/medarh.2017.71.169-172
Braga L, Pereira V, Cordeiro C, Moraes M, Araújo V, Dias M. Sofrimento psíquico em trabalhadores da estratégia saúde da família. Rev Enferm UFPE. 2013;7(2):345-54.
Cordioli DFC, Cordioli Junior JR, Gazetta CE, Silva AG, Lourenção LG. Occupational stress and engagement in primary health care workers. Rev Bras Enferm. 2019;72(6):1580-7. https://doi.org/10.1590/0034-7167-2018-0681 DOI: https://doi.org/10.1590/0034-7167-2018-0681
Garcia GPA, Marziale MHP. Satisfação, estresse e esgotamento profissional de enfermeiros gestores e assistencialistas da Atenção Primária à Saúde. Rev Esc Enferm USP. 2021;55:e03675. https://doi.org/10.1590/s1980-220x2019021503675 DOI: https://doi.org/10.1590/s1980-220x2019021503675
Ribeiro RP, Marziale MHP, Martins JT, Galdino MJQ, Ribeiro PHV. Estresse ocupacional entre trabalhadores de saúde de um hospital universitário. Rer Gaúcha Enferm. 2018;39:e65127. https://doi.org/10.1590/1983-1447.2018.65127 DOI: https://doi.org/10.1590/1983-1447.2018.65127
Vieira J, Anido I, Calife K. Mulheres profissionais da saúde e as repercussões da pandemia da COVID-19: é mais difícil para elas? Saude Debate. 2022;46(132):47-62. https://doi.org/10.1590/0103-1104202213203 DOI: https://doi.org/10.1590/0103-1104202213203
Fernandes JM, Moraes JCCA, Silva LADS, Nascimento MM, Preto VA. O estresse psicológico em relação ao sexo feminino e masculino no Brasil: uma revisão narrativa da literatura. Revista e-HUMANIT@S. 2019;6. Available from: https://bit.ly/42wFdbS
Macêdo ATS, Sousa MTD, Gomes RLM, Rolim MAB, Bastos JEP, Dantas RDSA, et al. Estresse Laboral em Profissionais da Saúde na Ambiência da Unidade de Terapia Intensiva. Id on Line Rev Mult Psic. 2018;12(42): 524-47. https://doi.org/10.14295/idonline.v12i42.1350 DOI: https://doi.org/10.14295/idonline.v12i42.1350
Roseno DA, Cavalcanti JRLP, Freire MAM. Caracterização da síndrome de burnout em enfermeiros em municípios do interior do Estado da Paraíba-Brasil. Rev Cienc Saude. 2020;10(1):23-30. https://doi.org/10.21876/rcshci.v10i1.877 DOI: https://doi.org/10.21876/rcshci.v10i1.877
Freitas CC, Freire MAM. Síndrome de Burnout em enfermeiros trabalhadores de um hospital público de Natal, Rio Grande do Norte, Brasil. Rev Cienc Saude. 2020;10(2):5-12. https://doi.org/10.21876/rcshci.v10i2.937 DOI: https://doi.org/10.21876/rcshci.v10i2.937
Teixeira CFDS, Soares CM, Souza EA, Lisboa ES, Pinto ICDM, Andrade LRD, Espiridião MA. A saúde dos profissionais de saúde no enfrentamento da pandemia de COVID-19. Cienc Saude Colet. 2020;25(9):3465-74. https://doi.org/10.1590/1413-81232020259.19562020 DOI: https://doi.org/10.1590/1413-81232020259.19562020
Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019-2021. JAMA network open. 2022;5(9): e2232748. https://doi.org/10.1001/jamanetworkopen.2022.32748 DOI: https://doi.org/10.1001/jamanetworkopen.2022.32748