Mortality trends due to Paracoccidioidomycosis in Brazil – 1996 to 2020
Main Article Content
Abstract
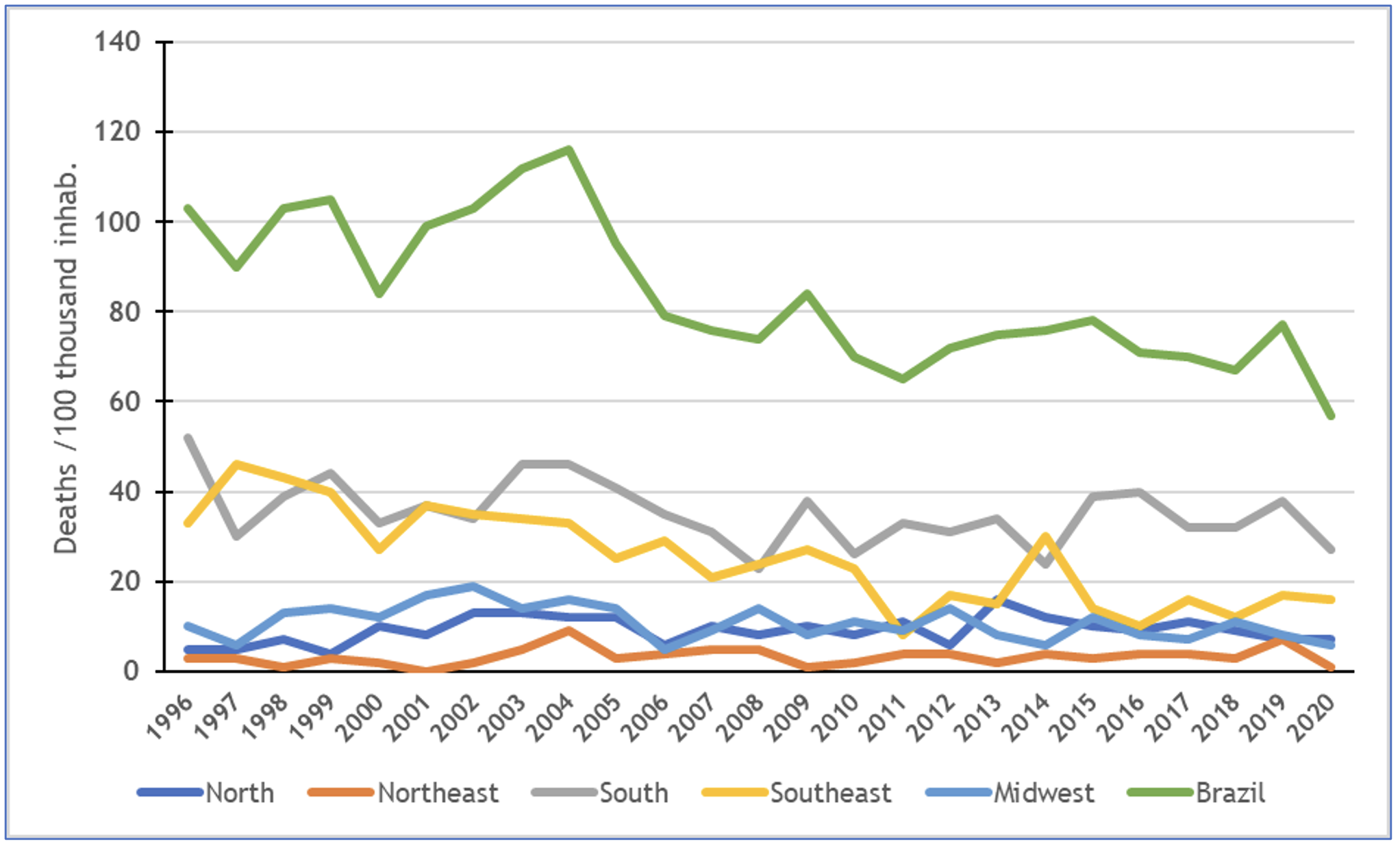
Objective: To analyze the trend in mortality from paracoccidioidomycosis (PCM) and characterize the sociodemographic profile in Brazil and its geographic regions in a 25-year time series. Methods: This is an ecological time series study. The study participants were the Brazilian population divided into age groups whose underlying cause of death was PCM. To calculate the annual percentage change (VPA) of the coefficients in the trend analysis, the Prais-Winsten regression was used. National mortality coefficients were calculated according to geographic regions, sex and age group and proportional to the other variables. Results: According to this study, there were 2,101 deaths from PCM in Brazil. The trend over the 25 years showed stable behavior in the North and Northeast regions. In the South, Southeast, and Midwest, there was a downward trend. The average mortality in Brazil was 84.04/100,000 inhab., VPA -3.29 (95% CI -2.43; -4.14). According to the analysis of sociodemographic aspects, there was a predominance of ignored schooling (764 deaths; 36%), white race/skin color (1,109; 53%), mixed marital status: married (942; 45%) and single (640; 30%), and place of death predominantly in the hospital environment (1,852; 88%). Conclusion: In Brazil and in the Southeast, South, andMidwest geographic regions, mortality from PCM showed a decreasing temporal trend. In the Northeast and North regions, the trend was stationary. The sociodemographic profile of the dying patients indicated males, adults, with low education, white, and married.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Bittencourt JIM, Oliveira RMD, Coutinho ZF. Mortalidade por paracoccidioidomicose no Estado do Paraná, Brasil, 1980/1998. Cad Saúde Pública. 2005;21(6):1856-64. https://doi.org/10.1590/S0102-311X2005000600035
Stringuini FA, Naback PO, Araújo LF, Lima RB, Martins CJ. Paracoccidioidomicose grave, com desfecho fatal e incidência relacionada a evento ambiental. An Bras Dermatol. 2023;98(1):133-7. https://doi.org/10.1016/j.abd.2021.12.006
Mendes RP, Cavalcante RS, Marques SA, Marques MEA, Venturini J, Sylvestre TF, et al. Paracoccidioidomycosis: Current Perspectives from Brazil. Open Microbiol J. 2017;11:224-282. https://doi.org/10.2174%2F1874285801711010224
Shikanai-Yasuda MA, Telles Filho FDQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39(3):297-310. https://doi.org/10.1590/S0037-86822006000300017
Coutinho ZF, Silva DD, Lazéra M, Petri V, Oliveira RMD, Sabroza PC, et al. Mortalidade por paracoccidioidomicose no Brasil (1980-1995). Cad Saude Publica. 2002;18(5):1441-54. https://doi.org/10.1590/S0102-311X2002000500037
Restrepo A, McEwen JG, Castañeda E. The habitat of Paracoccidioides brasiliensis: how far from solving the riddle? Med Mycol. 2001;39(3):233-41. https://doi.org/10.1080/mmy.39.3.233.241
Colombo AL, Tobón A, Restrepo A, Queiroz-Telles F, Nucci M. Epidemiology of endemic systemic fungal infections in Latin America. Med Mycol. 2011;49(8):785-98. https://doi.org/10.3109/13693786.2011.577821
Franco M, Bagagli E, Scapolio S, da Silva Lacaz C. A critical analysis of isolation of Paracoccidioides brasiliensis from soil. Med Mycol. 2000;38(3):185-91. https://doi.org/10.1080/mmy.38.3.185.191
Brasil. Ministério da Saúde. Paracoccidioidomicose. Governo do Brasil. Situação epidemiológica. [Internet]. [updated 3 Nov 2022; cited 14 Ago 2023]. Available from: https://bit.ly/45XPcb7
Lima-Costa MF, Barreto SM. Tipos de estudos epidemiológicos: conceitos básicos e aplicações na área do envelhecimento. Epidemiol Serv Saúde. 2003;12(4):189-201. https://doi.org/10.5123/S1679-49742003000400003
Landau EC, Moura L. Configuração territorial do Brasil: divisão política, biomas, características demográficas e socioeconômicas [livro]. Embrapa Brasil 50 anos; 2020 [cited 2023 Abr 21]. Available from: https://bit.ly/3Z4a664
Antunes JLF, Cardoso MRA. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol Serv Saúde. 2015;24(3):565-76. https://doi.org/10.5123/S1679-49742015000300024
Arruda VLD, Freitas BHBMD, Marcon SR, Fernandes FY, Lima NVPD, Bortolini J. Suicídio em adultos jovens brasileiros: série temporal de 1997 a 2019. Ciênc Saude Colet. 2021;26(07):2699-708. https://doi.org/10.1590/1413-81232021267.08502021
Leite MS, Silva ABG, Pestana BC, Ribeiro CDO, Caires DA, Oliveira EC, et al. Paracoccidioidomicose: relato de caso em mulher jovem sem fatores de risco. Braz J Surg Clin Res. 2020 [cited 5 Sep 2023];29(2):68-72. Available from: https://bit.ly/44GB05k
Coutinho, ZF. Morbimortalidade por paracoccidioidomicose no Brasil: 1998-2006 [Doctoral Thesis] [Portuguese]. Rio de Janeiro: Fundação Oswaldo Cruz. Escola Nacional de Saúde Pública Sergio Arouca. Programa de Pós-graduação em Saúde Pública; 2011 [cited 2023 Abr 21]. Available from: https://www.arca.fiocruz.br/handle/icict/23006
Palmeiro M, Cherubini K, Yurgel LS. Paracoccidioidomicose–revisão da literatura. Scientia Medica. 2005 [cited 2023 Abr 21];15(4):274-8. Available from: https://bit.ly/45Bch3J
Santos WAD, Silva BMD, Passos ED, Zandonade E, Falqueto A. Associação entre tabagismo e paracoccidioidomicose: um estudo de caso-controle no Estado do Espírito Santo, Brasil. Cad Saúde Pública. 2003;19(1):245-53. https://doi.org/10.1590/S0102-311X2003000100027
Campos MVS. Estudo de pacientes com paracoccidioidomicose e a coinfecção paracoccidioidomicose HIV/aids, assistidos no Hospital Universitário de Brasília entre 1984 e 2005 [Dissertação de Mestrado]. Brasília, DF: Universidade de Brasília, Faculdade de Medicina. Mestrado em Ciências Médicas; 2006 [cited 2023 Abr 21]. Available from: https://repositorio.unb.br/handle/10482/7995
Santo AH. Tendência da mortalidade relacionada à paracoccidioidomicose, Estado de São Paulo, Brasil, 1985 a 2005: estudo usando causas múltiplas de morte. Rev Panam Salud Pública. 2008 [cited 5 Sep 2023];23(5):313-24. Available from: https://bit.ly/3Z42O28
Buffara LT, Marques NK, Haag K, Steclan CA, Della AP, Nones DP, et al. Neuroparacoccidioidomicose em mulher adulta jovem: relato de caso. J Bras Neurocirur. 2021 [cited 2023 Abr 21]; 32(1): 89-94. Available from: https://bit.ly/3Z2fNBz
Bueno LMT. Influência do gênero na resposta dos neutrófilos contra a infecção por Paracoccidioides brasiliensis [Master’s Dissertation]. Ribeirão Preto: Programa de Pós-graduação em Biologia Celular e Molecular, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo;2018 [cited 2023 Abr 21]. https://doi.org/10.11606/D.17.2019.tde-15012019-095914
Fabris LR, Andrade ÚV, Santos AFD, Marques APDC, Oliveira SMDVLD, Mendes RP, et al. Prevalência decrescente da forma clínica aguda/subaguda da paracoccidioidomicose no Estado de Mato Grosso do Sul, Brasil. Rev Inst Med Trop São Paulo. 2014;56(2):121-5. https://doi.org/10.1590/S0036-46652014000200006
Carvalho R, Branquinho F, Theias R, Perloiro MDC. Paracoccidioidomicose Brasiliensis: a propósito de um caso clínico. Med Int. 2009 [cited 2023 Abr 21]; 16(3):170-2. Available from: https://revista.spmi.pt/index.php/rpmi/article/view/1416
Alvares BA, Gracia CAL, Marques MEA, Marque SA. Paracoccidioidomicose: manifestação clínica incomum. An Bras Dermatol. 2020 [cited 2023 Abr 21]; 95(6):740-742. https://doi.org/10.1016/j.abd.2020.06.001
Palheta-Neto FX, Moreira JS, Martins ACDC, Cruz FJ, Gomes, ER, Pezzin-Palheta AC. Estudo de 26 casos de Paracoccidioidomicose avaliados no Serviço de Otorrinolaringologia da Fundação Oswaldo Cruz (FIOCRUZ).Rev Bras Otorrinolaringol. 2003;69(5):622-7. https://doi.org/10.1590/S0034-72992003000500006
Bellissimo-Rodrigues F, Bollela VB, Fonseca BAL, Martinez R. Endemic paracoccidioidomycosis: relationship between clinical presentation and patients’ demographic features. Med Mycol. 2013;51(3):313–18. https://doi.org/10.3109/13693786.2012.714529
Martinez R. New Trends in Paracoccidioidomycosis Epidemiology. J Fungi (Basel). 2017;3(1):1. https://doi.org/10.3390/jof3010001