Analysis of the breathing function in wind instrumental musicians
Main Article Content
Abstract
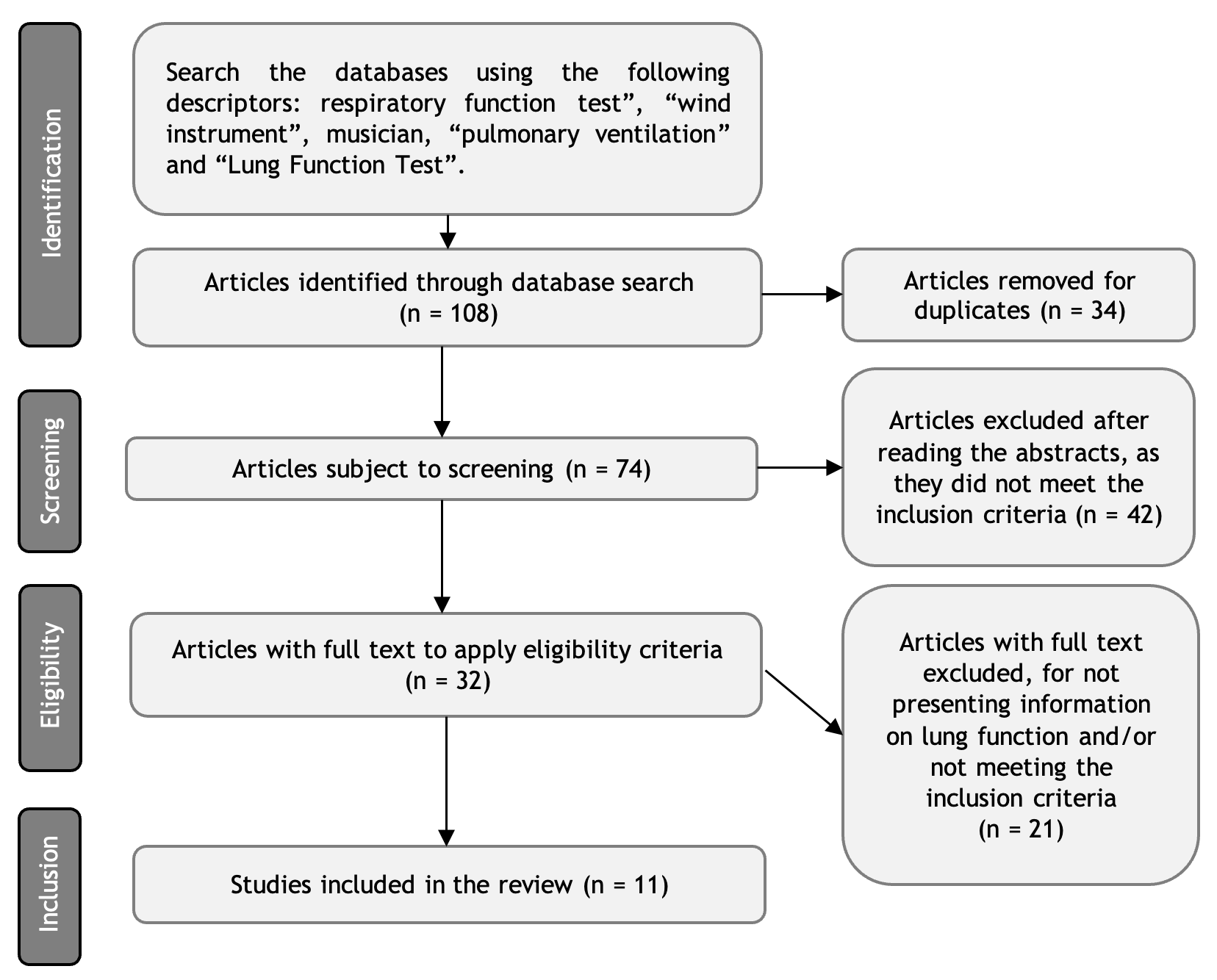
Objective: To conduct an integrative review of lung function and respiratory muscle strength in wind instrument musicians. The relationship between respiratory function and the use of wind musical instruments is an area of knowledge that has not been extensively explored. Methods: A bibliographic review was carried out in the MEDLINE, Embase, Cochrane, PeDro, BVS, Scopus, Web of Science, and SciELO databases by combining the keywords “respiratory function test”, “wind instrument”, musician, “pulmonary ventilation” and “Lung Function Test”. Results: Initially, 108 articles were found, of which 11 were selected, totaling 596 wind instrumentalists who were part of the study groups. In most studies, musicians showed lower values of expired volume in one second (FEV1) and forced vital capacity (FVC) in spirometry than in the control group. However, there was no difference regarding the FEV1/FVC ratio, just as there was no difference in respiratory muscle strength or relationship with respiratory diseases. Conclusion: Current studies regarding the effect of wind instruments on individuals are unable to show positive or negative impacts on the respiratory health of this population.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Fuhrmann AG, Franklin PJ, Hall GL. Prolonged use of wind or brass instruments does not alter lung function in musicians. Respir Med. 2011;105(5):761-7. https://doi.org/10.1016/j.rmed.2011.01.017
Wolfe J. The acoustics of woodwind musical instruments. Acoust Today. 2018;14(1):50-6. Available from: https://bit.ly/3Pw7hI3
Lima JMA. Abrem-se as cortinas: O som da Orquestra e seus Instrumentos. Música na Educação Básica. 2017;4(4). Available from: https://bit.ly/3Pvn5uq
Wolfe J, Fletcher NH, Smith J. The Interactions Between Wind Instruments and their Players. Acta Acustica united with Acustica. 2015;101(2):211-23. https://doi.org/10.3813/AAA.918820
Ponce MC, Sankari A, Sharma S. Pulmonary Function Tests. 2022 Sep 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 29493964.
Smith J, Kreisman H, Colacone A, Fox J, Wolkove N. Sensation of inspired volumes and pressures in professional wind instrument players. J Appl Physiol (1985). 1990;68(6):2380-3. https://doi.org/10.1152/jappl.1990.68.6.2380
Khuje PD, Hulke SM. Comparative study of pulmonary functions of clarinet and trumpet players. Res J Pharm Biol Chem Sci. 2012;3(2):746-51.
Antoniadou M, Michaelidis V, Tsara V. Lung function in wind instrument players. Pneumon [Internet]. 2012 [cited 7 Sep 2023];25(2):180-3. Available from: https://bit.ly/485RGpG
Marshall B, Levy S. Microbial contamination of musical wind instruments. Int J Environ Health Res. 2011;21(4):275-85. https://doi.org/10.1080/09603123.2010.550033
Deniz O, Savci S, Tozkoparan E, Ince DI, Ucar M, Ciftci F. Reduced pulmonary function in wind instrument players. Arch Med Res. 2006;37(4):506-10. https://doi.org/10.1016/j.arcmed.2005.09.015
Subramanian RK, Joshua SDR, Saikumar P, Marthandam LJ. Estimation of lung functions and risk of developing obstructive sleep apnoea in wind instrument players. Indian J Physiol. Pharmaco. 2018;62(1):59-65. https://doi.org/10.1007/s11818-015-0714-0
Studer L, Schumann DM, Stalder-Siebeneichler A, Tamm M, Stolz D. Does trumpet playing affect lung function? A case-control study. PLoS One. 2019;14(5):e0215781. https://doi.org/10.1371/journal.pone.0215781
Hahnengress ML, Böning D. Cardiopulmonary changes during clarinet playing. Eur J Appl Physiol. 2010;110(6):1199-208. https://doi.org/10.1007/s00421-010-1576-6
Brzęk A, Famuła A, Kowalczyk A, Plinta R. Efficiency of lung ventilation for people performing wind instruments. Med Pr. 2016;67(4):427-33. https://doi.org/10.13075/mp.5893.00398
Granell J, Granell J, Ruiz D, Tapias JA. El estudio de instrumentos de viento se asocia con un patrón obstructivo en la espirometría de adolescentes con buena capacidad de resistencia aeróbica. Aten Primaria. 2011;43(3):134-9. https://doi.org/10.1016/j.aprim.2010.03.013
Soria SS, Castello JR, García AV, García AC, Martínez AC. Expiratory flow in wind musicians, application to the consideration of distances against COVID-19. Invest Clin (Venezuela). 2021;62(1):16-27. https://doi.org/10.22209/IC.v62n1a02
Schorr-Lesnick B, Teirstein AS, Brown LK, Miller A. Pulmonary function in singers and wind-instrument players. Chest. 1985;88(2):201-5. https://doi.org/10.1378/chest.88.2.201
Fuhrmann A, Wijsman S, Weinstein P, Poulsen D, Franklin P. Asthma among musicians in Australia: is there a difference between wind/brass and other players?. Med Probl Perf Art. 2009; 24(4):170-4. https://doi.org/10.21091/mppa.2009.4034