Incidence of infections associated with the use of invasive devices in an ICU after application of the Improvement Science Method
Main Article Content
Abstract
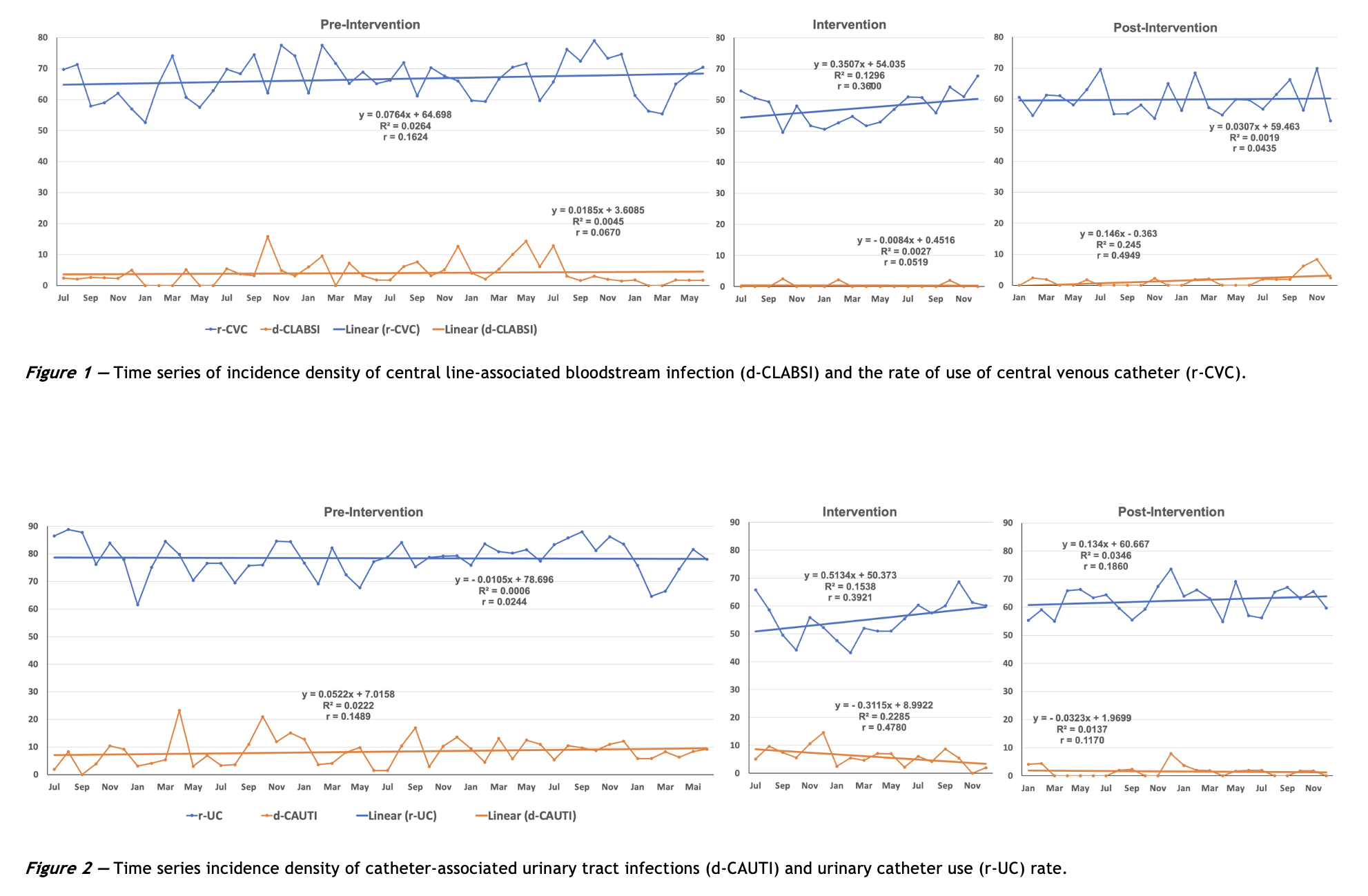
Objective: To reduce the incidence density of ventilator-associated pneumonia (VAP), central line-associated bloodstream infection (CLABSI), and catheter-associated urinary tract infection (CAUTI) in the intensive care unit (ICU) using the Improvement Science method. Methods: This was a single-center retrospective cohort study. A collaborative quality improvement team developed and implemented local changes to HAI-related processes and protocols. Pre-intervention, intervention, and post-intervention periods were compared. The study was conducted at the Adult ICU of a hospital in southern Brazil. Variables were analyzed using interrupted time series analysis with segmented linear regression, simple correlation, and hypothesis testing. Results: There was a reduction in the incidence density of all infections. VAP was reduced from 27.2% to 7.2% (p < 0.001), CLABSI from 3.0% to 0.9% (p = 0.017), and CAUTI from 8.3% to 1.8% (p < 0.001). The ICU stay was also reduced from 6.7 to 6 days (p = 0.018). Conclusion: There was an improvement in all the evaluated parameters. Ongoing monitoring of related indicators and adherence to implemented measures are essential to sustain improvements. Applying the Improvement Science methodology can reduce the incidence of HAIs in the ICU.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Allegranzi B, Bagheri Nejad S, Combescure C, Attar H, Donaldson L, Pittet D. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377: 228-41. https://doi.org/10.1016/S0140-6736(10)61458-4
Burke JP. Infection control - a problem for patient safety. N Engl J Med. 2003;348(7):651-6. https://doi.org/10.1056/NEJMhpr020557
Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections [published correction appears in N Engl J Med. 2022 16 Jun;386(24):2348. N Engl J Med. 2014;370(13):1198-208. https://doi.org/10.1056/NEJMoa1306801
Strich JR, Palmore TN. Preventing Transmission of Multidrug-Resistant Pathogens in the Intensive Care Unit. Infect Dis Clin North Am. 2017;31(3):535-50; https://doi.org/10.1016/j.idc.2017.05.010
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323-29. https://doi.org/10.1001/jama.2009.1754
Ylipalosaari P, Ala-Kokko TI, Laurila J, Ohtonen P, Syrjälä H. Intensive care acquired infection is an independent risk factor for hospital mortality: a prospective cohort study. Crit Care. 2006;10(2):R66. https://doi.org/10.1186/cc4902
Garland A. Improving the ICU: part 1. Chest. 2005;127(6):2151-64; https://doi.org/10.1378/chest.127.6.2151
Garland A. Improving the ICU: part 2. Chest. 2005; 127(6):2165-79; https://doi.org/10.1378/chest.127.6.2165
Mauger B, Marbella A, Pines E, Chopra R, Black ER, Aronson N. Implementing quality improvement strategies to reduce healthcare-associated infections: A systematic review. Am J Infect Control. 2014;42(10 Suppl):S274-83; https://doi.org/10.1016/j.ajic.2014.05.031
Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008;337:a1714; https://doi.org/10.1136/bmj.a1714
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500-59. https://doi.org/10.1111/j.1468-0009.2010.00611.x
Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153(10):1423-31.
Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ. 2001;323(7315):746-9. https://doi.org/10.1136/bmj.323.7315.746
Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500-59. https://doi.org/10.1111/j.1468-0009.2010.00611.x
Courtlandt CD, Noonan L, Feld LG. Model for improvement - Part 1: A framework for health care quality. Pediatr Clin North Am. 2009;56(4):757-78. https://doi.org/10.1016/j.pcl.2009.06.002
Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Wiley; 2009.
IHI Innovation White Paper. The breakthrough series: IHI's collaborative model for achieving breakthrough improvement. Boston: Institute for Health Improvement; 2003. Available at: https://bit.ly/3sSrFKs
Randolph G, Esporas M, Provost L, Massie S, Bundy DG. Model for improvement - Part Two: Measurement and feedback for quality improvement efforts. Pediatr Clin North Am. 2009;56(4):779-98. https://doi.org/10.1016/j.pcl.2009.05.012
Hospital Nossa Senhora da Conceição. Tubarão. Accessed 09 Mar, 2022. Available at: https://bit.ly/3PCRarS
IBGE. Panorama da cidade de Tubarão-SC. Accessed 12 Sep 2023. Available at: https://bit.ly/45LvHmz
Agência Nacional de Vigilância Sanitária. Critérios Diagnósticos de Infecção Relacionada à Assistência à Saúde. Série: Segurança do Paciente e Qualidade em Serviços de Saúde. Brasília; 2013. Accessed 9 Sep 2023. Available at: https://bit.ly/455uMMF
Gandra S, Ellison RT 3rd. Modern trends in infection control practices in intensive care units. J Intensive Care Med. 2014;29(6):311-26. https://doi.org/10.1177/0885066613485215
Dudeck MA, Horan TC, Peterson KD, et al. National Healthcare Safety Network (NHSN) report, data summary for 2009, device-associated module. Am J Infect Control. 2011;39(5):349-67. https://doi.org/10.1016/j.ajic.2011.04.011
Watson SR, Scales DC. Improving intensive care unit quality using collaborative networks. Crit Care Clin. 2013;29(1):77-89. https://doi.org/10.1016/j.ccc.2012.10.008
Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review. BMJ Qual Saf. 2018;27(3):226-40; https://doi.org/10.1136/bmjqs-2017-006926
Centers For Disease Control and Prevention. NHSN Surveillance Definitions for Specific Types of Infections. Atlanta (US): CDC; 2014.
Rosenthal VD, Desse J, Maurizi DM, Chaparro GJ, Orellano PW, Chediack V, et al. Impact of the International Nosocomial Infection Control Consortium's multidimensional approach on rates of ventilator-associated pneumonia in 14 intensive care units in 11 hospitals of 5 cities within Argentina. Am J Infect Control. 2018; 46:674-9; https://doi.org/10.1016/j.ajic.2017.11.021
Schechner V, Wulffhart L, Temkin E, Feldman SF, Nutman A, Shitrit P, et al. One-year mortality and years of potential life lost following bloodstream infection among adults: A nation-wide population based study. Lancet Reg Health Eur. 2022;23:100511. https://doi.org/10.1016/j.lanepe.2022.100511
Ista E, van der Hoven B, Kornelisse RF, van der Starre C, Vos MC, Boersma E, et al. Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(6):724-34. https://doi.org/10.1016/S1473-3099(15)00409-0
Shadle HN, Sabol V, Smith A, Stafford H, Thompson JA, Bowers M. A Bundle-Based Approach to Prevent Catheter-Associated Urinary Tract Infections in the Intensive Care Unit. Crit Care Nurse. 2021;41(2):62-71. https://doi.org/10.4037/ccn2021934