Strategies used by Primary Care Nurses in the prevention of cervical cancer: integrative review
Main Article Content
Abstract
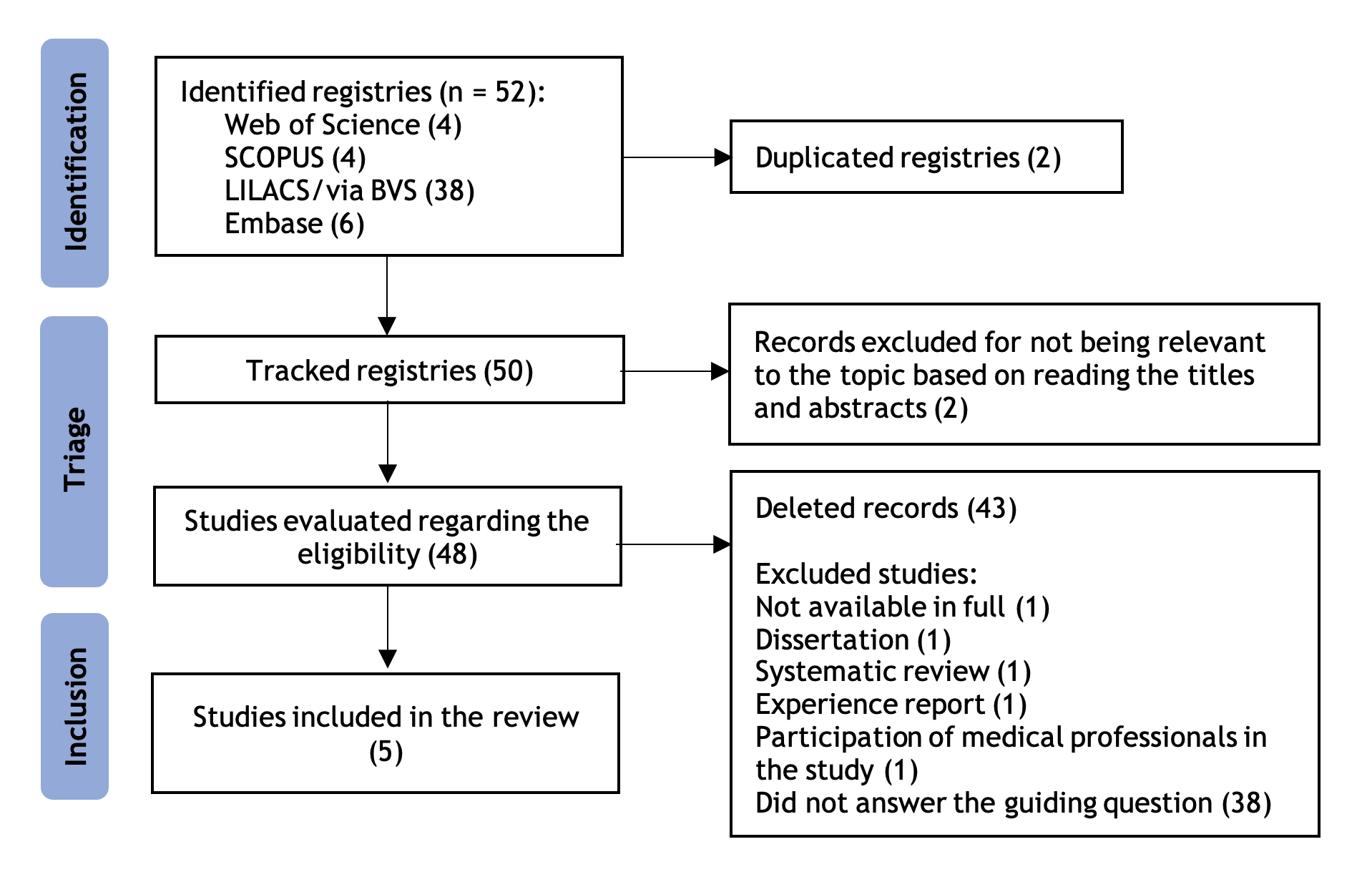
Objective: to identify, in the scientific literature, the strategies used by primary care nurses to prevent cervical cancer. Methods: An integrative review of the EMBASE, LILACS (BVS), SCOPUS, and Web of Science databases between March and April 2023. After the search, the selected articles were read in full, and the data were extracted for analysis. The final sample consisted of 5 studies. Results: the main strategies used were educational interventions, with a predominance of lectures and subsequent invitations or collection of material to carry out the preventive exam. Conversation circles (culture circles), telephone guidance, and the provision of a self-completed clinical form during the nursing consultation were also used. Conclusions: the studies made it possible to identify positive strategies for preventing cervical cancer, which could direct nurses to increasingly invest in methodologies aimed at increasing women’s autonomy.
men.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
2. Cerqueira RS, Santos HLPC, Prado NMBL, Bittencourt RG, Biscarde DGDS, Santos AM. Controle do câncer do colo do útero na atenção primária à saúde em países sul-americanos: revisão sistemática. Rev Panam Salud Publica. 2022 Aug 18;46:e107. https://doi.org/10.26633%2FRPSP.2022.107
3. Carvalho KF, Costa LMO, França RF. A relação entre HPV e Câncer de Colo de Útero: um panorama a partir da produção bibliográfica da área. Revista Saúde em Foco [Internet]. 2019 [cited 2023 Mar 20];11(5):1-15. Available from: https://portal.unisepe.com.br/unifia/wp-content/uploads/sites/10001/2019/02/021_A-RELA%C3%87%C3%83O-ENTRE-HPV-E-C%C3%82NCER-DE-COLO-DE-%C3%9ATERO-UM-PANORAMA-A-PARTIR-DA-PRODU%C3%87%C3%83O-BIBLIOGR%C3%81FICA-DA-%C3%81REA.pdf
4. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Coordenação de Prevenção e Vigilância. Divisão de Vigilância e Análise de Situação. Estimativa 2023: incidência de câncer no Brasil [Internet]. Rio de Janeiro: INCA; 2023 [cited 2023 Jul 20]. Available from: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//estimativa-2023.pdf
5. Ministério da Saúde (BR). Recomendações do INCA para reduzir a mortalidade por câncer de mama no Brasil [Internet]. Brasília: Instituto Nacional do Câncer; 2023 [cited 2023 Jun 20]. Available from: https://www.inca.gov.br/publicacoes/folhetos/recomendacoes-do-inca-para-reduzir-mortalidade-por-cancer-de-mama-no-brasil
6. Silva LG, Andrade GO, Leonhardt V, Bezerra MLR. A importância da prevenção do câncer de colo do útero: revisão integrativa. Res., Soc. Dev. 2021;10(15):e533101523334. http://dx.doi.org/10.33448/rsd-v10i1 5.23334
7. Pecinato V, Jacobo A, Silva SG. Mortality trends of breast and cervical cancer in Passo Fundo, Rio Grande do Sul: an analysis by age and schooling, 1999-2019. Epidemiol. Serv. Saúde. 2022;31(3):1-14. https://doi.org/10.1590/S2237-96222022000300021
8. Anjos EF, Andrade KB, Martins PC, Paiva JAC, Prado NMBL, Santos AM. Professionals’ practice and quality of actions to control cervical cancer: a cross-sectional study. Esc. Anna Nery Rev. Enferm. 2022;26:e20210137. https://doi.org/10.1590/2177-9465-ean-2021-0137
9. Maciel NS, Luzia FJM, Ferreira DS, Ferreira LCC, Mendonça VM, Oliveira AWN, et al. Active search toincrease adherenceto the pap smear test. Rev. Enferm. UFPE on line. 2021;15:e245678. https://doi.org/10.5205/1981-8963.2021.245678
10. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005 Dec;52(5):546-53. https://doi.org/10.1111/j.1365-2648.2005.03621.x
11. Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis [Internet]. Adelaide: Joanna Briggs Institute; 2020 [cited 2021 Aug 6]. Available from: https://jbi-global-wiki.refined.site/space/MANUAL/4688637/Chapter+2%3A+Systematic+reviews+of+qualitative+evidence
12. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan — a web and mobile app for systematic reviews. Syst. Rev. 2016 Dec;5(1):210. http://dx.doi.org/10.1186/s13643-016-0384-4
13. Correio KDL, Ramos AIG, Santos RLG, Bushatsky M, Correio MBSCB. Control of cervical cancer: actions taken by nurses based on collective subject discourse. Rev. Pesqui. (Univ. Fed. Estado Rio J., Online). 2015;7(2):2425-39. https://doi.org/10.9789/2175-5361.2015.v7i2.2425-2439
14. Lima TM, Nicolau AIO, Carvalho FHC, Vasconcelos CTM, Aquino PS, Pinheiro AKB. Telephone interventions for adherenceto colpocytological examination. Rev. Latinoam. Enferm. 2017;25:e2844. https://doi.org/10.1590/1518-8345.1683.2844
15. Nepomuceno CC, Fernandes BM, Almeida MIG, Freitas SC, Bertocchi FM. Auto preenchimento da ficha clínica no rastreamento do câncer de colo uterino: percepções da mulher. Rev. Enferm. Cent.-Oeste Min. 2015;5(1):1401-10. https://doi.org/10.19175/recom.v0i0.825
16. Vasconcelos CTM, Pinheiro AKB, Nicolau AIO, Lima TM, Barbosa DFF. Comparison among the efficacy of interventions for the return rate to receive the pap test report: randomized controlled clinical trial. Rev. Latinoam. Enferm. 2017;25:e2857. https://doi.org/10.1590/1518-8345.1337.2857
17. Dias EG, Carvalho BC, Alves NS, Caldeira MB, Teixeira JAL. Atuação do enfermeiro na prevenção do câncer do colo de útero em Unidades de Saúde. J. Health Biol. Sci. 2021;9(1):1-6. http://dx.doi.org/10.12662/2317-3076jhbs.v9i1.3472.p1-6.2021
18. Silva GA, Alcantara LLM, Tomazelli JG, Ribeiro CM, Girianelli VR, Santos ÉC, et al. Avaliação das ações de controle do câncer de colo do útero no Brasil e regiões a partir dos dados registrados no Sistema Único de Saúde. Cad. Saúde Pública. 2022;38(7). https://doi.org/10.1590/0102-311xpt041722
19. Oliveira RL, Lima LAS, Ramos LGA. A. Assistência do enfermeiro na educação em saúde, no câncer de colo do útero. Research, Society and Development. 2021, 10(4). http://dx.doi.org/10.33448/rsd-v10i4.13728
20. Ferreccio C. Nuevas estrategias de prevención y control de cáncer de cuello uterino en Chile. Salud Publica Mex. 2018 Nov-Dic;60(6):713-21. https://doi.org/10.21149/8577
21. Melo EMF. A importância da realização do exame preventivo em mulheres acima dos 40 anos. Saúde Colet. [Internet]. 2011 [cited 2023 Jan 10];8(54):249-52. Available from: www.redalyc.org/pdf/842/84221108006.pdf
22. Ministério da Saúde (BR). Portaria de Consolidação no 2, de 28 de setembro de 2017. Consolidação das normas sobre as políticas nacionais de saúde do Sistema Único de Saúde [Internet]. Brasília, DF; 2017 [cited 2020 May 10]. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prc0002_03_10_2017.html
23. Reis TCR, Figueiredo MFS, Souza LPS, Silva JR, Amaral AKM, Messias RB, et al. Educação em saúde: aspectos históricos no Brasil. J Health Sci Inst [Internet]. 2013 [cited 2023 Mar 20];31(2):219-23. Available from: https://repositorio.unip.br/wp-content/uploads/2020/12/V31_n2_2013_p219a223.pdf
24. Freire P. Pedagogia do oprimido. Rio de Janeiro: Paz e Terra; 1978.
25. Fittipaldi ALM, O’Dwyer G, Henriques P. Educação em saúde na atenção primária: as abordagens e estratégias contempladas nas políticas públicas de saúde. Interface (Botucatu, Online). 2021;25:e200806. https://doi.org/10.1590/interface.200806
26. Souza ACC, Moreira TMM, Borges JWP. Educational technologies designed to promote cardiovascular health in adults: integrative review. Rev. Esc. Enferm. USP. 2014 Oct;48(5):941-8. https://doi.org/10.1590/s0080-6234201400005000023
27. Silveira MS, Cogo ALP. The contributions of digital technologies in the teaching of nursing skills: an integrative review. Rev. Gaúch. Enferm. 2017;38(2):e66204. https://doi.org/10.1590/1983-1447.2017.02.66204
28. Lavender T, Richens Y, Milan SJ, Smyth RMD, Dowswell T. Telephone support for women during pregnancy and the first six weeks postpartum. Cochrane Database Syst. Rev. 2013 Jul 18;(7):CD009338. https://doi.org/10.1002/14651858.cd009338.pub2
29. Oriá MOB, Dodou HD, Chaves AFL, Santos LMDA, Ximenes LB, Vasceoncelos CTM. Effectiveness of educational interventions conducted by telephone to promote breastfeeding: a systematic review of the literature. Rev. Esc. Enferm. USP. 2018;52:e03333. https://doi.org/10.1590/S1980-220X2017024303333
30. Moretto IG, Contim CLV, Espírito Santo FH. Telephone follow-up as a nursing intervention for patients receiving outpatient chemotherapy: integrative review. Rev. Gaúch. Enferm. 2019;40:e20190039. https://doi.org/10.1590/1983-1447.2019.20190039
31. Machado TMD, Santana RF, Hercules ABS. Telecare central: nursing intervention perspective. Cogitare Enferm. 2020;25:e66666. http://dx.doi.org/10.5380/ce.v25i0.66666
32. Becker TAC. O acompanhamento por telefone como estratégia de intervenção de3 enfermagem no processo de aplicação de insulina no domicílio [Dissertação de Mestrado]. Ribeirão Preto: Universidade de São Paulo; 2010 [cited 2023 Mar 22]. Available from: https://www.teses.usp.br/teses/disponiveis/22/22132/tde-16112010-111054/pt-br.php
33. Santos JN, Gomes RS. Women’s Feelings and Perceptions about Cervical Cancer Preventive Practices: Integrative Literature Review. Rev. Bras. Cancerol. 2022;68(2):e-031632. https://doi.org/10.32635/2176-9745.RBC.2022v68n2.1632
34. Freire P. À sombra desta mangueira. São Paulo: Olho d’Água; 1995.
35. Heidemann ITSB, Almeida MCP. Freire’s dialogic concept enables family health program teams to incorporate health promotion. Public Health Nurs. 2011 Mar-Apr;28(2):159-67. https://doi.org/10.1111/j.1525-1446.2010.00898.x.