Adherence to Heart Rate Training Zones in an Exercise Training Program in Adults with Coronary Artery Disease
Main Article Content
Abstract
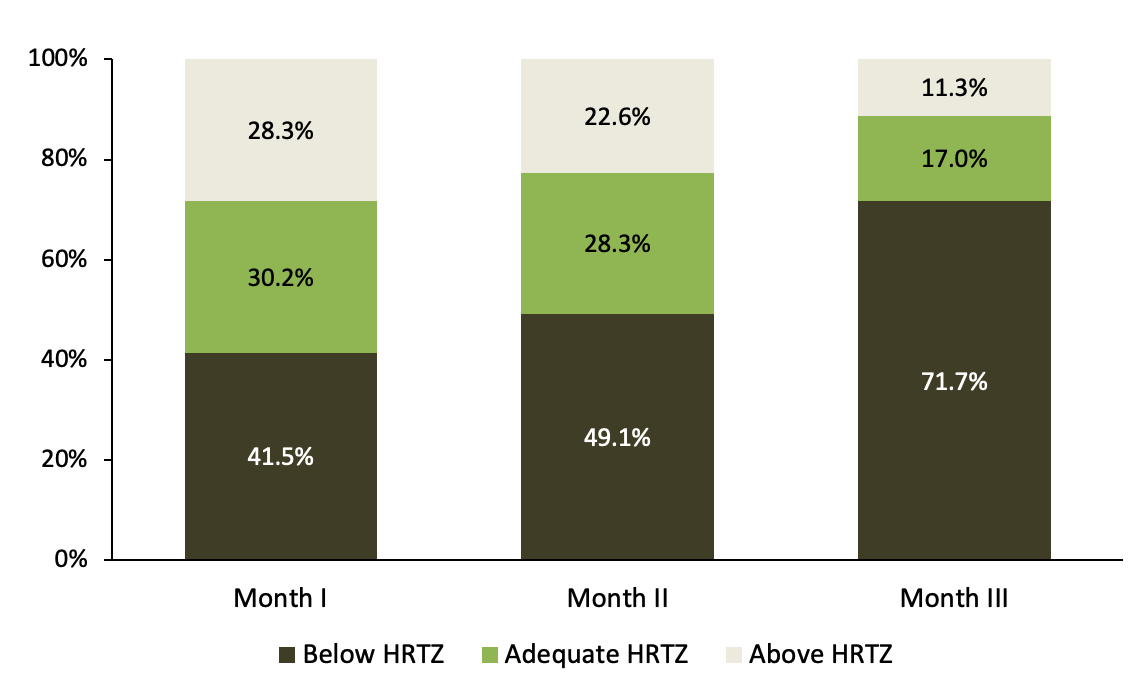
Objectives: To investigate the effect of exercise intensity on functional capacity in individuals with coronary artery disease, assess adherence to the heart rate training zone (HRTZ), and determine the relationship between trained intensity and functional capacity. Methods: A retrospective study was conducted on the medical records of 54 outpatients with coronary artery disease in a public hospital. The prescribed intensity started at 50%–60% of the heart rate reserve, increasing monthly to 70%–80% by the third month. Spearman’s test was used to assess the correlation between improvement in distance in the incremental shuttle walk test (ISWT), exercise intensity, and rating of perceived exertion (Borg–RPE). Adherence was classified as ‘below’ when HRTZ was not achieved in any phase of the program, ‘intermediate’ when HR was within the HRTZ for one or two months, and ‘above’ when HR was at or higher than HRTZ ≥ two months. Improvement was tested using t-test and one-way ANOVA. Results: 51.9% of participants had an increase in ISWT of ≥70 m (p < 0.0001). In at least one month, 50.9% trained below HRTZ. The trained intensity did not fall below 8.6% of the prescribed HRTZ minimum threshold. Changes in ISWT were not significantly correlated with exercise intensity (p = 0.87) or Borg–RPE (p = 0.16). Conclusion: While a significant increase in functional capacity was found, considerable heterogeneity in changes were observed. This may, in part, be related to adherence to HRTZ with progressive exercise intensity and to the variability in exercise volume in cardiovascular rehabilitation programs.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Abell B, Glasziou P, Hoffmann T. The Contribution of Individual Exercise Training Components to Clinical Outcomes in Randomised Controlled Trials of Cardiac Rehabilitation: A Systematic Review and Meta-regression. Sports Med Open. 2017;3(1):19. https://doi.org/10.1186/s40798-017-0086-z PMid:28477308 PMCid:PMC5419959 DOI: https://doi.org/10.1186/s40798-017-0086-z
Epstein E, Rosander A, Pazargadi A, Taub P. Cardiac Rehab for Functional Improvement. Curr Heart Fail Rep. 2020;17(4):161-70. https://doi.org/10.1007/s11897-020-00462-2 PMid:32514659 DOI: https://doi.org/10.1007/s11897-020-00462-2
Ozemek C, Arena R, Rouleau CR, Campbell TS, Hauer T, Wilton SB, et al. Long-Term Maintenance of Cardiorespiratory Fitness Gains After Cardiac Rehabilitation Reduces Mortality Risk in Patients With Multimorbidity. J Cardiopulm Rehabil Prev. 2023;43(2):109-14. https://doi.org/10.1097/HCR.0000000000000734 PMid:36203224 DOI: https://doi.org/10.1097/HCR.0000000000000734
Hung RK, Al-Mallah MH, McEvoy JW, Whelton SP, Blumenthal RS, Nasir K, et al. Prognostic value of exercise capacity in patients with coronary artery disease: the FIT (Henry Ford ExercIse Testing) project. Mayo Clin Proc. 2014;89(12):1644-54. https://doi.org/10.1016/j.mayocp.2014.07.011 PMid:25440889 DOI: https://doi.org/10.1016/j.mayocp.2014.07.011
Vromen T, Spee RF, Kraal JJ, Peek N, van Engen-Verheul MM, Kraaijenhagen RA, et al. Exercise training programs in Dutch cardiac rehabilitation centres. Neth Heart J. 2013;21(3):138-43. https://doi.org/10.1007/s12471-013-0374-2 PMid:23338553 PMCid:PMC3578523 DOI: https://doi.org/10.1007/s12471-013-0374-2
Abell B, Glasziou P, Briffa T, Hoffmann T. Exercise training characteristics in cardiac rehabilitation programmes: a cross-sectional survey of Australian practice. Open Heart. 2016;3(1):374. https://doi.org/10.1136/openhrt-2015-000374 PMid:27127639 PMCid:PMC4847132 DOI: https://doi.org/10.1136/openhrt-2015-000374
Hansen D, Rovelo Ruiz G, Doherty P, Iliou MC, Vromen T, Hinton S, et al. Do clinicians prescribe exercise similarly in patients with different cardiovascular diseases? Findings from the EAPC EXPERT working group survey. Eur J Prev Cardiol. 2018;25(7):682-91. https://doi.org/10.1177/2047487318760888 PMid:29486587 DOI: https://doi.org/10.1177/2047487318760888
Khushhal A, Nichols S, Carroll S, Abt G, Ingle L. Insufficient exercise intensity for clinical benefit? Monitoring and quantification of a community-based Phase III cardiac rehabilitation programme: A United Kingdom perspective. PLoS One. 2019;14(6):e0217654. https://doi.org/10.1371/journal.pone.0217654 PMid:31194759 PMCid:PMC6563987 DOI: https://doi.org/10.1371/journal.pone.0217654
Ismail H, McFarlane JR, Dieberg G, Smart NA. Exercise training program characteristics and magnitude of change in functional capacity of heart failure patients. Int J Cardiol. 2014;171(1):62-5. https://doi.org/10.1016/j.ijcard.2013.11.045 PMid:24326210 DOI: https://doi.org/10.1016/j.ijcard.2013.11.045
Taylor JL, Bonikowske AR, Olson TP. Optimizing Outcomes in Cardiac Rehabilitation: The Importance of Exercise Intensity. Front Cardiovasc Med. 2021;8:734278. https://doi.org/10.3389/fcvm.2021.734278 PMid:34540924 PMCid:PMC8446279 DOI: https://doi.org/10.3389/fcvm.2021.734278
Li WG, Huang Z, Zhang XA. Exercise prescription in cardiac rehabilitation needs to be more accurate. Eur J Prev Cardiol. 2021;28(7):e33-4. https://doi.org/10.1177/2047487320936021 DOI: https://doi.org/10.1177/2047487320936021
Grace SL, Midence L, Oh P, Brister S, Chessex C, Stewart DE, et al. Cardiac Rehabilitation Program Adherence and Functional Capacity Among Women: A Randomized Controlled Trial. Mayo Clin Proc. 2016;91(2):140-8. https://doi.org/10.1016/j.mayocp.2015.10.021 PMid:26682921 DOI: https://doi.org/10.1016/j.mayocp.2015.10.021
Meneghelo RS, Araújo CGS, Stein R, Mastrocolla LE, Albuquerque PF, Serra SM. III Diretrizes da Sociedade Brasileira de Cardiologia sobre teste ergométrico. Arq. Bras. Cardiol. 2010;95(1):1-30. https://doi.org/10.1590/S0066-782X2010002400001 DOI: https://doi.org/10.1590/S0066-782X2010002400001
Schwaab B, Bjarnason-Wehrens B, Meng K, Albus C, Salzwedel A, Schmid JP, et al. Cardiac Rehabilitation in German Speaking Countries of Europe-Evidence-Based Guidelines from Germany, Austria and Switzerland LLKardReha-DACH-Part 2. J Clin Med. 2021;10(14):3071. https://doi.org/10.3390/jcm10143071 PMid:34300237 PMCid:PMC8306118 DOI: https://doi.org/10.3390/jcm10143071
Herdy AH, López-Jiménez F, Terzic CP, Milani M, Stein R, Carvalho T, et al. South American guidelines for cardiovascular disease prevention and rehabilitation. Arq Bras Cardiol. 2014;103(2 Suppl 1):1-31. https://doi.org/10.5935/abc.2014S003 PMid:25387466 DOI: https://doi.org/10.5935/abc.2014S003
Borg G. The Borg CR10 Scale. Borg's perceived exertion and pain scales. 1st ed. Human Kinetics; 1998.
Scherr J, Wolfarth B, Christle JW, Pressler A, Wagenpfeil S, Halle M. Associations between Borg's rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113(1):147-55. https://doi.org/10.1007/s00421-012-2421-x PMid:22615009 DOI: https://doi.org/10.1007/s00421-012-2421-x
Lelis JD, Chaves G, Ghisi GLM, Grace SL, Britto RR. Validity of the Incremental Shuttle Walk Test to Assess Exercise Safety When Initiating Cardiac Rehabilitation in Low-Resource Settings. J Cardiopulm Rehabil Prev. 2019;39(3):E1-7. https://doi.org/10.1097/HCR.0000000000000412 PMid:31022005 DOI: https://doi.org/10.1097/HCR.0000000000000412
Monteiro DP, Britto RR, Carvalho MLV, Montemezzo D, Parreira VF, Pereira DAG. Shuttle walking test como instrumento de avaliação da capacidade funcional: uma revisão da literatura. Cienc Saude. 2014;7(2):92-7. https://doi.org/10.15448/1983-652X.2014.2.16580 DOI: https://doi.org/10.15448/1983-652X.2014.2.16580
Maranhão-Neto GDA, Leon ACPD, Farinatti PDTV. Validade e equivalência da versão em português do Veterans Specific Activity Questionnaire. Arq Bras Cardiol. 2011;97:130-5. https://doi.org/10.1590/S0066-782X2011005000071 PMid:21670897 DOI: https://doi.org/10.1590/S0066-782X2011005000071
Houchen-Wolloff L, Boyce S, Singh S. The minimum clinically important improvement in the incremental shuttle walk test following cardiac rehabilitation. Eur J Prev Cardiol. 2015;22(8):972-8. https://doi.org/10.1177/2047487314540840 PMid:24958737 DOI: https://doi.org/10.1177/2047487314540840
Mitchell BL, Lock MJ, Davison K, Parfitt G, Buckley JP, Eston RG. What is the effect of aerobic exercise intensity on cardiorespiratory fitness in those undergoing cardiac rehabilitation? A systematic review with meta-analysis. Br J Sports Med. 2018;53(21):1341-51. https://doi.org/10.1136/bjsports-2018-099153 PMid:30121584 DOI: https://doi.org/10.1136/bjsports-2018-099153
Amorim H, Cadilha R, Parada F, Rocha A. Progression of aerobic exercise intensity in a cardiac rehabilitation program. Rev Port Cardiol (Engl Ed). 2019;38(4):281-6. https://doi.org/10.1016/j.repc.2018.07.009 PMid:31109760 DOI: https://doi.org/10.1016/j.repc.2018.07.009