Support provided by healthcare professionals to the mothers of newborns in the neonatal unit
Conteúdo do artigo principal
Resumo
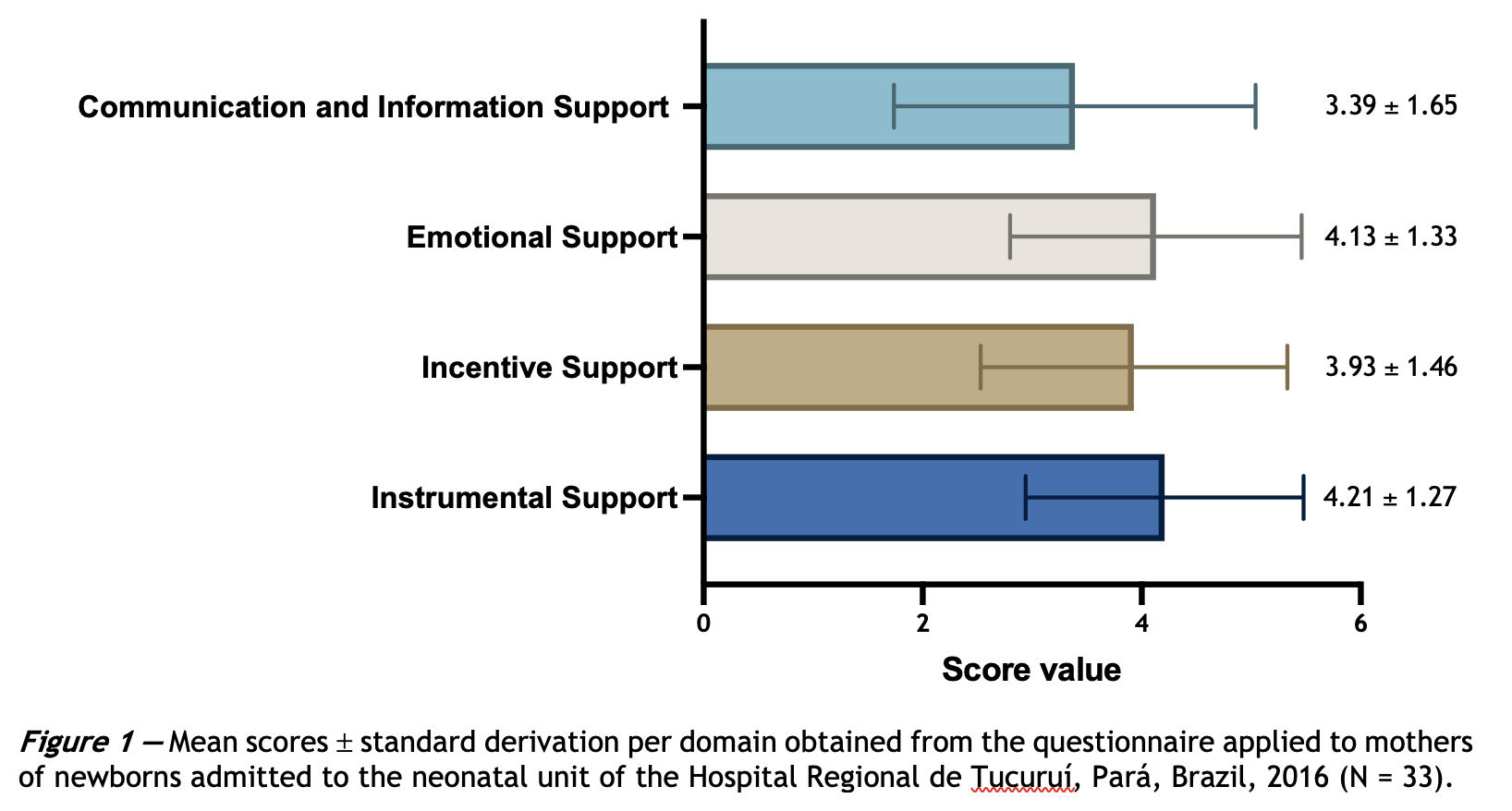
Objective: To evaluate the support offered by health professionals to mothers of newborns admitted to the neonatal unit.Methods: Descriptive cross-sectional study with a quantitative approach conducted at the Regional Hospital of Tucuruí, in the state of Pará, region of the Brazilian Amazon, where 33 mothers who had newborn children admitted to the neonatal unit responded to the structured adapted version of the NPST (Nurse Parent Support Tool ). Results: Most were aged 20-34 years (48%), married or in a stable relationship (69%), multiracial (87%), housewife (57%), with up to 11 years of study (72%). The scores for the NPST subdomains were 3.39 ± 1.65 (Communication and Information Support), 4.13 ± 1.33 (Emotional Support), 3.93 ± 1.46 (Incentive Support), and 4.21 ± 1,27 (Instrumental Support). The findings revealed unsatisfactory communication and information support from health professionals to mothers, although they expressed satisfaction with the care provided. Conclusions: The perception of scarcity of human resources and health education, verified in this study, weakens the communication process during hospitalization and influences the mother's well-being, leading to a decrease in the efficiency of the support provided. The improvement in this area can lead to better results in daily practice. The replication of this study to other locations can lead to more significant assistance to mothers of hospitalized neonates and provide new technologies and strategies in health education.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
Kegler JJ, Neves ET, Silva AM, Jantsch LB, Bertoldo CS, Silva JH. Stress in parents of newborns in a neonatal intensive care unit. Esc Anna Nery. 2019;23(1): e20180178. https://doi.org/10.1590/2177-9465-ean-2018-0178
Rolim K, Santiago N, Vieira T, Sancho M, Frota M, Boulard H, et al. Imaginário de mães acerca da hospitalização do filho na unidade de terapia intensiva neonatal. Enferm Foco. 2016;7(1):42-46. https://doi.org/10.21675/2357-707X.2016.v7.n1.664
Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014;27(17):1738-43. https://doi.org/10.3109/14767058.2014.942626 PMid:25005861
Ramos FP, Enumo SRF, Paula KMP. Maternal coping with baby hospitalization at a neonatal intensive care unit. Paideia. 2017;27(67):10-9. https://doi.org/10.1590/1982-43272767201702
Yaman S, Altay N. Posttraumatic stress and experiences of parents with a newborn in the neonatal intensive care unit. J Reprod Infant Psychol. 2015;33(2):140-52. https://doi.org/10.1080/02646838.2014.990872
Nayeri UA, Buhimschi CS, Zhao G, Buhimschi IA, Bhandari V. Components of the antepartum, intrapartum, and postpartum exposome impact on distinct short-term adverse neonatal outcomes of premature infants: A prospective cohort study. PLoS One. 2018;13(12):e0207298. https://doi.org/10.1371/journal.pone.0207298 PMid:30517142 PMCid:PMC6281222
Figueiredo JV, Fialho AVM, Mendonça GMM, Rodrigues DP, Silva LFD. Pain in the immediate puerperium: nursing care contribution. Rev Bras Enferm. 2018;71(suppl 3):1343-50. https://doi.org/10.1590/0034-7167-2017-0345 PMid:29972533
Brasil. Ministério da Saúde. Política Nacional de Humanização [Internet]. Brasília, DF: Ministério da Saúde; 2013 [cited 2021 May 22]. Avaiable from: https://bit.ly/3oGslMY
Naidon ÂM, Neves ET, Silveira A da, Ribeiro CF. Gestation, delivery, birth and hospitalization of newborns in neonatal intensive therapy: mother's report. Texto Context Enferm. 2019;27(2):e5750016. https://doi.org/10.1590/0104-070720180005750016
Brasil, Ministério da Economia, Instituto Brasileiro de Geografia e Estatística. Síntese de Indicadores Sociais 2020. Rio de Janeiro, RJ: IBGE; 2020 [cited 2021 May 22]. Avaiable from: https://bit.ly/3bNFNt7
Brasil, Ministério da Saúde. Secretaria Executiva e Saúde Pública. Tucuruí. 2020.
Miles MS, Carlson J, Brunssen S. The nurse parent support tool. J Pediatr Nurs. 1999;14(1):44-50. https://doi.org/10.1016/S0882-5963(99)80059-1
Rossetto EG, Martins TB, Mejias NA. Adaptação transcultural e validação do instrumento nurse parent support tool para a língua portuguesa. Online Brazilian J Nurs. 2011;10(2):1-10. https://doi.org/10.5935/1676-4285.20113305
Dias BF, Antoni N, Vargas D. Clinical and epidemiological profile of pregnancy in adolescence: an ecological study. Arq Catarinenses Med [Internet]. 2020 [cited 2021 May 9];49(1):10-22. Avaiable from: https://bit.ly/3f2Fxaw
Aldrighi JD, Wall ML, Souza SR, Cancela FZ. The experiences of pregnant women at an advanced maternal age: an integrative review. Rev Esc Enferm USP. 2016;50(3):512-21. https://doi.org/10.1590/S0080-623420160000400019 PMid:27556724
Mendes Costa RL, Pereira dos Santos AA, Torres de Lima Sanches ME. Assessement of the profile of assisted women during the obstetric risk classification process. Rev Pesq Cuid Fundam Online. 2019;11(2):488-94. https://doi.org/10.9789/2175-5361.2019.v11i2.488-494
Souza WPS, Maia EMC, Oliveira MAM, Morais TIS, Cardoso PS, Lira ECS, et al. Gravidez tardia: relações entre características sociodemográficas, gestacionais e apoio social. Bol Psicol [Internet]. 2016 [cited 2021 May 9];66(144):47-59. Avaiable from: https://bit.ly/2SuP820
Henz GS, Medeiros CRG, Salvadori M. A inclusão paterna durante o pré-natal. Rev Enferm Atenção Saúde. 2017;6(1):52-66. https://doi.org/10.18554/reas.v6i1.2053
Luz RT, Trindade TBS, Lima DS, Climaco LCC, Ferraz IS, Teixeira SCR, et al. Importância da presença dos pais durante o internamento neonatal. Rev Enferm UFPE on line. 2019;13:e239790. https://doi.org/10.5205/1981-8963.2019.239790
Reynolds L, Duncan M, Smith G, Matur A, Neil J, Inder T, et al. Parental presence and holding in the neonatal intensive care unit and associations with early neurobehavior. J Perinatol. 2013;33:636–41. https://doi.org/10.1038/jp.2013.4
Franck LS, Axelin A. Differences in parents', nurses' and physicians' views of NICU parent support. Acta Paediatr. 2013;102(6):590-6. https://doi.org/10.1111/apa.12227
Aftyka A, Rozalska-Walaszek I, Wróbel A, Bednarek A, Dąbek K, Zarzycka D. Support provided by nurses to parents of hospitalized children - cultural adaptation and validation of Nurse Parent Support Tool and initial research results. Scand J Caring Sci. 2017;31(4):1012-21. https://doi.org/10.1111/scs.12426
Akkoyun S, Tas Arslan F. Investigation of stress and nursing support in mothers of preterm infants in neonatal intensive care units. Scand J Caring Sci. 2019;33(2):351-8. https://doi.org/10.1111/scs.12630
Araújo BBM, Rodrigues BMRD, de Araújo Pacheco ST. A promoção do cuidado materno ao neonato prematuro: A perspectiva da educação problematizadora em saúde. Rev Enferm. 2015;23(1):128-31. https://doi.org/10.12957/reuerj.2015.14779
Mattos A, Jacó-Vilela AM, Mendes DMF, Ribeiro HFC, Hernandez JG, Quadros LCT, et al. Vivências e expectativas de mães com recém-nascidos pré-termo internados em unidade de terapia intensiva neonatal. Estud Pesqui Psicol. 2019;19(3):562-5. https://doi.org/10.12957/epp.2019.47078
Rossetto EG, Martins TB, Mejias NA. Satisfação Dos pais em relação aos cuidados de enfermagem numa unidade de cuidados intensivos e especiais neonatais e pediátricos - Aplicação da Escala de Apoio dos Enfermeiros aos Pais – Versão Portuguesa da Nurse Parent Support Tool, Na Ucienp Do Hospit. Rev Clin Hosp Prof Dr Fernando Fonseca. 2016;4(1/2):14-19. https://doi.org/10.5935/1676-4285.20113305
Donabedian A. Prioridades para el progreso en la evaluación y monitoreo de la calidad de la atención. Salud Publica Mex. 1993;35(1):94-7. Spanish. PMID: 8470025
Costa DGD, Moura GMSS, Moraes MG, Santos JLGD, Magalhães AMM. Satisfaction attributes related to safety and quality perceived in the experience of hospitalized patients. Rev Gaucha Enferm. 2019;41(spe):e20190152. https://doi.org/10.1590/1983-1447.2020.20190152 PMid:31778385
Melo RA, Araújo AKC, Marques WF, Santos NM, Fernandes FECV, Bezerra CS. Sentimentos de mães de recém-nascidos internados em uma unidade de terapia intensiva neonatal. Id on Line Rev Psic. 2016;10(32):88-103. https://doi.org/10.14295/idonline.v10i32.569
Pinheiro MR, Carr AMG. A eficácia do método mãe canguru em comparação aos cuidados convencionais em uma UTI Neonatal. Braz J Heal Rev [Internet]. 2019 [cited 2021 may 22];2(2):1039-48. Avaiable fom: https://bit.ly/34azk72
Akashi H, Ishioka M, Hagiwara A, Akashi R, Osanai Y. Core factors promoting a continuum of care for maternal, newborn, and child health in Japan. Biosci Trends. 2018;12(1):1-6. https://doi.org/10.5582/bst.2017.01304 PMid:29479018
Kikuchi K, Yasuoka J, Nanishi K, Ahmed A, Nohara Y, Nishikitani M, et al. Postnatal care could be the key to improving the continuum of care in maternal and child health in Ratanakiri, Cambodia. PLoS One. 2018;13(6):e0198829. https://doi.org/10.1371/journal.pone.0198829 PMid:29889894 PMCid:PMC5995361
Freire LM, Camponêz PSP, Maciel IVL, Vieira CS, Bueno M, Duarte ED. Factors associated with non-adherence to outpatient follow-up of neonatal intensive care discharge. Rev Esc Enferm USP. 2018;52:e03372. https://doi.org/10.1590/s1980-220x2017029703372 PMid:30517296
Mok E, Leung SF. Nurses as providers of support for mothers of premature infants. J Clin Nurs. 2006;15(6):726-34. https://doi.org/10.1111/j.1365-2702.2006.01359.x PMID:16684168.
Valizadeh L, Zamanzadeh V, Akbarbegloo M, Sayadi L. Importance and availability of nursing support for mothers in NICU: A comparison of opinions of Iranian mothers and nurses. Iran J Pediatr. 2012;22(2):191-6. PMID:23056885 PMCID:PMC3446074.