A relação do excesso de peso com a infertilidade feminina
Conteúdo do artigo principal
Resumo
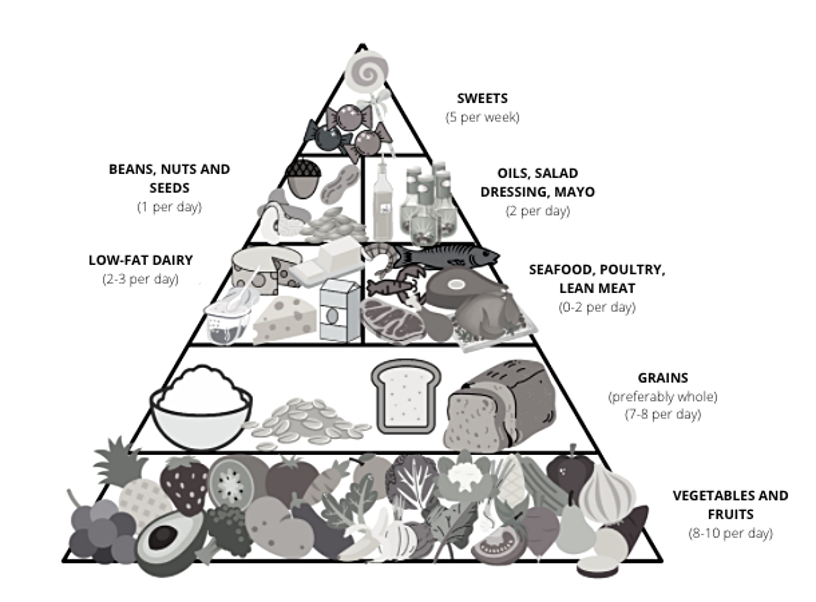
O excesso de peso parece influenciar negativamente na fertilidade e, por ser um fator modificável, a compreensão sobre essa relação pode contribuir para o tratamento da infertilidade. O tecido adiposo é responsável pela liberação de diversos hormônios e citocinas relacionados ao sistema reprodutor, como leptina, FNT-a e Interleucina-6. A obesidade está relacionada com a resistência à insulina e ao hiperandrogenismo ovariano, fatores que podem gerar impacto negativo na fertilidade feminina. Além disso, a dieta e o estilo de vida da mulher podem influenciar o peso corporal e a fertilidade. O consumo alimentar caracterizado pela elevada ingestão de alimentos com alta densidade energética, elevados teores de açúcar, gordura saturada e pobre em nutrientes, assim como a inatividade física, favorece o excesso de peso. A perda de peso corporal obtida por meio de uma alimentação saudável associada à prática de atividade física pode ser capaz de restaurar a fertilidade.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
Lashen H. Investigations for infertility. Obstet Gynaecol Reprod Med. 2007;17(7): 211-6. https://doi.org/10.1016/j.ogrm.2007.05.002
Silvestris E, Lovero D, Palmirotta R. Nutrition and female fertility: an interdependent correlation. Front Endocrinol (Lausanne). 2019;10:346. https://doi.org/10.3389/fendo.2019.00346 PMid:31231310 PMCid:PMC6568019
Sociedade Brasileira de Reprodução Assistida [Internet]. Movimento da Fertilidade [cited 2021 Nov 20]. Avaiable from: https://bit.ly/3DFbIYG
Frey KA, Patel KS. Initial evaluation and management of infertility by the primary care physician. Mayo Clin Proc. 2004 Nov;79(11):1439-43; quiz 1443. https://doi.org/10.4065/79.11.1439 PMid:15544024
Brasil, Ministério da Saúde, Vigitel Brasil 2019: Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico [Internet]. Brasília, DF: Ministério da Saúde; 2020 [cited 2021 Nov 20]. Avaiable from: https://bit.ly/3vsWmkQ
Oliveira JB. Obesity and Reproduction. JBRA Assist Reprod. 2016;20(4):194. https://doi.org/10.5935/1518-0557.20160037 PMid:28050951 PMCid:PMC5265615
Fichman V, Costa RS, Miglioli TC, Marinheiro LP. Association of obesity and anovulatory infertility. Einstein (Sao Paulo). 2020;18:eAO5150 https://doi.org/10.31744/einstein_journal/2020AO5150 PMid:32159605 PMCid:PMC7053827
World Health Organization Obesity and overweight [Internet]. New York: WHO [update 2021 Jun 21; cited 2021 Nov 20]. Avaiable from: https://bit.ly/3nCjQ6k
Giviziez CR, Sanchez EG, Approbato MS, Maia MC, Fleury EA, Sasaki RS. Obesity and anovulatory infertility: A review. JBRA Assist Reprod. 2016;20(4):240-5. https://doi.org/10.5935/1518-0557.20160046 PMid:28050960 PMCid:PMC5265624
Pasquali R, Patton L, Gambineri A. Obesity and infertility. Curr Opin Endocrinol Diabetes Obes. 2007;14(6):482-7. https://doi.org/10.1097/MED.0b013e3282f1d6cb PMid:17982356
Broughton DE, Moley KH. Obesity and female infertility: potential mediators of obesity's impact. Fertil Steril. 2017;107(4):840-7. https://doi.org/10.1016/j.fertnstert.2017.01.017 PMid:28292619
Gambineri A, Laudisio D, Marocco C, Radellini S, Colao A, Savastano S; Obesity Programs of nutrition, Education, Research and Assessment (OPERA) group. Female infertility: which role for obesity? Int J Obes Suppl. 2019;9(1):65-72. https://doi.org/10.1038/s41367-019-0009-1 PMid:31391925 PMCid:PMC6683114
Koga F, Kitagami S, Izumi A, Uemura T, Takayama O, Koga T, Mizoguchi T. Relationship between nutrition and reproduction. Reprod Med Biol. 2020;19(3):254-64. https://doi.org/10.1002/rmb2.12332 PMid:32684824 PMCid:PMC7360971
Martin M Matzuk, Dolores JL. The biology of infertility: research advances and clinical challenges. Nat Med. 2008;14(6):1197-213. https://doi.org/10.1038/nm.f.1895 PMid:18989307 PMCid:PMC3786590
Dağ ZÖ, Dilbaz B. Impact of obesity on infertility in women. J Turk Ger Gynecol Assoc. 2015;16(2):111-7. https://doi.org/10.5152/jtgga.2015.15232 PMid:26097395 PMCid:PMC4456969
Costa EC, Soares EM, Lemos TM, Maranhão TM, Azevedo GD. Índices de obesidade central e fatores de risco cardiovascular na síndrome dos ovários policísticos. Arq Bras Cardiol. 2010;94(5):633-8 [Portuguese]. https://doi.org/10.1590/S0066-782X2010005000029 PMid:20428724
Federação Brasileira das Associações de Ginecologia e Obstetrícia (FEBRASGO). Síndrome dos ovários policísticos. São Paulo: Febrasgo; 2018.
Rehme MF, Pontes AG, Corrente JE, Franco JG Jr, Pontes A. Contribuição do hiperandrogenismo para o desenvolvimento de síndrome metabólica em mulheres obesas com síndrome dos ovários policísticos. Rev Bras Ginecol Obstet. 2013;35(12):562-8 [Portuguese]. https://doi.org/10.1590/S0100-72032013001200006 PMid:24500511
Panth N, Gavarkovs A, Tamez M, Mattei J. The influence of diet on fertility and the implications for public health nutrition in the United States. Front Public Health. 2018;6:211. https://doi.org/10.3389/fpubh.2018.00211 PMid:30109221 PMCid:PMC6079277
American Congress of Obstetricians and Gynecologists. ACOG Committee Opinion No. 462: moderate caffeine consumption during pregnancy. Obstet Gynecol. 2010;116(2 Pt 1): 467-8. https://doi.org/10.1097/AOG.0b013e3181eeb2a1 PMid:20664420
Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35(2):158-76. https://doi.org/10.1016/j.amepre.2008.04.009 PMid:18617085 PMCid:PMC4465757
Coutinho JG, Gentil PC, Toral N. A desnutrição e obesidade no Brasil: o enfrentamento com base na agenda única da nutrição. Cad Saúde Pública. 2008;24(2):332-40. https://doi.org/10.1590/S0102-311X2008001400018 PMid:18670713
González Rodríguez LG, López Sobaler AM, Perea Sánchez JM, Ortega RM. Nutrición y fertilidade. Nutr. Hosp. 2018;35(Spec No6):7-10. [Spanish] https://doi.org/10.20960/nh.2279 PMid:30351153
Legro RS, Dodson WC, Kris-Etherton PM, Kunselman AR, Stetter CM, Williams NI et al. Randomized controlled trial of preconception interventions in infertile women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015;100(11):4048-58. https://doi.org/10.1210/jc.2015-2778 PMid:26401593 PMCid:PMC4702450
Teitelman M, Grotegut CA, Williams NN, Lewis JD. The impact of bariatric surgery on menstrual patterns. Obes Surg. 2006;16(11):1457-63. https://doi.org/10.1381/096089206778870148 PMid:17132411
Cucó G, Fernández-Ballart J, Sala J, Viladrich C, Iranzo R, Vila J, et al. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr. 2006;60(3):364-71. https://doi.org/10.1038/sj.ejcn.1602324 PMid:16340954
Jahangirifar M, Taebi M, Nasr-Esfahani MH, Askari GH. Dietary patterns and the outcomes of assisted reproductive techniques in women with primary infertility: a prospective cohort study. Int J Fertil Steril. 2019;12(4):316-23. https://doi.org/10.22074/ijfs.2019.5373 PMid:30291693 PMCid:PMC6186288
Azadi-Yazdi M, Karimi-Zarchi M , Salehi-Abargouei A ,Fallahzadeh H, Nadjarzadeh A. Effects of Dietary Approach to Stop Hypertension diet on androgens, antioxidant status and body composition in overweight and obese women with polycystic ovary syndrome: a randomised controlled trial. J Hum Nutr Diet. 2017;30(3):275-83. https://doi.org/10.1111/jhn.12433 PMid:28466507
Appel JL, Moore TJ, Obarzanek E, Vollmer WM, Svetkley LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117-24. https://doi.org/10.1056/NEJM199704173361601 PMid:9099655
Cambiaghi AS, Rosa DS. Fertilidade e alimentação: Guia alimentar para homens e mulheres que desejam preservar ou melhorar sua fertilidade. 1st ed. São Paulo: La Vida; 2012. 310 p. ISBN: 8598127183.
Fontana R, Della Torre S. The deep correlation between energy metabolism and reproduction: a view on the effects of nutrition for women fertility. Nutrients. 2016;8(2):87. https://doi.org/10.3390/nu8020087 PMid:26875986 PMCid:PMC4772050
Marcelino G, Hiane PA, Freitas KC, Santana LF, Pott A, Donadon JR et al. Efects of olive oil and its minor components on cardiovascular diseases, inflammation, and gut microbiota. Nutrients. 2019;11(8):1826. https://doi.org/10.3390/nu11081826 PMid:31394805 PMCid:PMC6722810
Willet CW, Sacks F, Trichopoulou A, Dresher G, Ferro-Luzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Nutr. 1995;61(suppl 1):S1402-6. https://doi.org/10.1093/ajcn/61.6.1402S PMid:7754995
Vujkovic M, de Vries JH, Lindemans J, Macklon NS, van der Spek PJ, Steegers EA, Steegers-Theunissen RP. The preconception Mediterranean dietary pattern in couples undergoing in vitro fertilization/intracytoplasmic sperm injection treatment increases the chance of pregnancy. Fertil Steril. 2010;94(6):2096-101. https://doi.org/10.1016/j.fertnstert.2009.12.079 PMid:20189169
Toledo E, Lopez-del Burgo C, Ruiz-Zambrana A, Donazar M, Navarro-Blasco I, Martínez-González MA, de Irala J. Dietary patterns and difficulty conceiving: a nested case-control study. Fertil Steril. 2011;96(5):1149-53. https://doi.org/10.1016/j.fertnstert.2011.08.034 PMid:21943725
Sakhaei R, Shahvazi S, Mozaffari-Khosravi H, Samadi M, Khatibi N, Nadjarzadeh A, Zare F, Salehi-Abargouei A. The Dietary Approaches to Stop Hypertension (DASH)-Style Diet and an alternative mediterranean diet are differently associated with serum inflammatory markers in female adults. Food Nutr Bull. 2018;39(3):361-76. https://doi.org/10.1177/0379572118783950 PMid:29969908
Estruch R, Martinez-Gonzalez MA, Corella DD, Basora-Gallisá J, Ruiz-Gutiérrez V, et al. Effects of dietary fibre intake on risk factors for cardiovascular disease in subjects at high risk. J Epidemiol Community Health. 2009;63(7):582-8. https://doi.org/10.1136/jech.2008.082214 PMid:19289389
Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. 2011;141(6):1083-8. https://doi.org/10.3945/jn.110.136739 PMid:21525259 PMCid:PMC3137257
Asemi Z, Esmaillzadeh A. DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Horm Metab Res. 2015;47(3):232-8. https://doi.org/10.1055/s-0034-1376990 PMid:24956415
Christina G Campbell, Blakely D Brown, Danielle Dufner, William G Thorland. Effects of soy or milk protein durign a high-fat feeding challenge on oxidative stress, inflammation, and lipids in healthy men. Lipids. 2006;41(3):257-65. https://doi.org/10.1007/s11745-006-5095-5 PMid:16711600