Associação entre terapia nutricional e complicações em pacientes diagnosticados com COVID-19 acompanhados no estado de Pernambuco
Conteúdo do artigo principal
Resumo
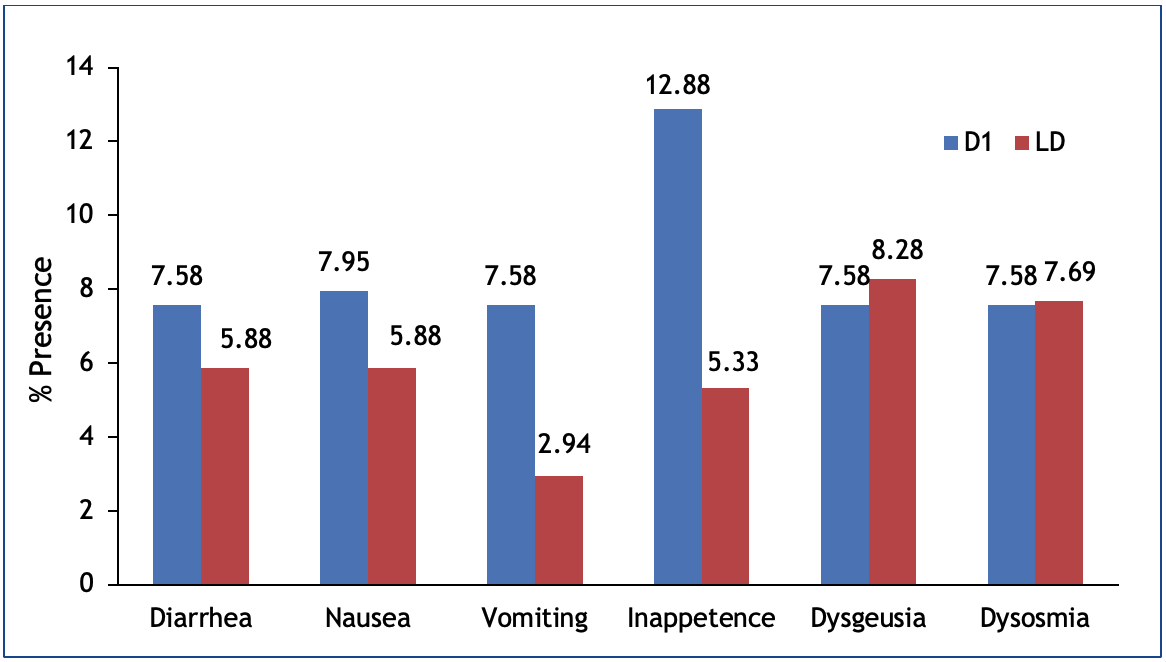
Objetivo: Analisar a associação entre terapia nutricional e complicações em pacientes diagnosticados com COVID-19 acompanhados no estado de Pernambuco. Métodos: Estudo do tipo coorte prospectiva, realizado a partir da análise de dados secundários de pesquisa multicêntrica, de junho de 2020 a junho de 2021. Foram incluídos pacientes de ambos os sexos, maiores de 18 anos, hospitalizados por COVID-19 em enfermarias e/ou unidades de terapia intensiva de oito hospitais. Foram coletados dados sociodemográficos e econômicos, de estado nutricional, terapia nutricional, complicações gastrointestinais e desfecho clínico, durante a admissão e término do internamento. Resultados: A amostra foi composta por 272 pacientes, com uma idade mediana de 67 anos (IIQ 54 - 76), distribuindo-se de forma semelhante entre homens e mulheres (50,4% vs. 49,6%). Foi observada uma maior frequência de sobrepeso/obesidade (40,31%). Inapetência (12,88%) e disgeusia (8,28%) foram as alterações mais frequentes. Foi observado que 84,6% receberam dieta precoce, a adequação calórica variou entre 72,1% e 60,7%, a via oral entre 82,4% e 70,7%, a maioria (58%) recebeu até 1,3 g de proteína ao dia e 46,7% foram a óbito. A adequação calórica se associou a disgeusia (p = 0,040) e desfecho clínico (p = 0,044) e apresentou tendência de associação ao vômito (p = 0,077). Não se encontrou associação com as proteínas. Conclusão: A terapia nutricional está associada a sintomas gastrointestinais, como vômitos e disgeusia e ao desfecho clínico dos pacientes com COVID-19.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
Machhi J, Herskovitz J, Senan AM, Dutta D, Nath B, Oleynikov MD, et al. The Natural History, Pathobiology, and Clinical Manifestations of SARS-CoV-2 Infections. J Neuroimmune Pharmacol. 2020;15(3):359-86. https://doi.org/10.1007/s11481-020-09944-5
Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020;14(2):185-92. https://doi.org/10.1007/s11684-020-0754-0
Iser BPM, Silva I, Raymundo VT, Poleto MB, Schuelter-Trevisol F, Bobinski F. Suspected COVID-19 case definition: a narrative review of the most frequent signs and symptoms among confirmed cases. Epidemiol Serv Saúde. 2020;29(3):e2020233. https://doi.org/10.5123/S1679-49742020000300018
Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27(5):1451-4. https://doi.org/10.1038/s41418-020-0530-3
Gomes DF, Gandolfo AS, De Oliveira AC, Potenza ALS, Micelli CLO, Almeida CB, et al. "Say No to Child Malnutrition" Campaign 11: important steps to fight hospital malnutrition. Braspen J. 2019;34(1):3-23.
Iddir M, Brito A, Dingeo G, Del Campo SSF, Samouda H, La Frano MR, Bohn T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12(6):1562. https://doi.org/10.3390/nu12061562
Associação Brasileira de Empresas e Pesquisa. Critério de Classificação Econômica Brasil. Alterações na aplicação do Critério Brasil. 2021.Available from: https://www.abep.org/criterio-brasil
World Health Organization - WHO. Physical status: the use and interpretation of anthropometry: Report of a WHO Expert Committee. Technical Report Series nº 854. Geneva: World Health Organization; 1995.
Organización Panamericana de la Salud. División de Promoción y Protección de la Salud (HPP). Encuesta Multicentrica salud beinestar y envejecimiento (SABE) em América Latina el Caribe: Informe Preliminar. In: XXXVI Reunión del Comité asesor de investigaciones em Salud; 9-11 jun 2001; Kingston, Jamaica: OPAS, 2002.
Beserra EA, Rodrigues PA, Lisboa AQ. Validação de métodos subjetivos para estimativa do índice de massa corporal em pacientes acamados. Com Ciências Saúde. 2011;22(1):19-26.
Campos LF, Barreto PA, Ceniccola GD, Gonçalves RC, De Matos LBN, Zambelli CMSF, et al. Review of the BRASPEN technical report on nutritional therapy in patients hospitalized with COVID-19. Braspen J. 2021;36(1):122-6.
Nunes AP, Zanchim MC, Kümpel DA, Rodrigues TP, Zanin J. Caloric-protein adequacy of enteral nutritional therapy in critically ill patients of a highly complex hospital in Rio Grande do Sul. Braspen J. 2018;33(2):116-21.
Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002-19. https://doi.org/10.1136/gutjnl-2020-320926
Zarifian A, Bidary MZ, Arekhi S, Rafiee M, Gholamalizadeh H, Amiriani A, et al. Gastrointestinal and hepatic abnormalities in patients with confirmed COVID-19: A systematic review and meta-analysis. J Med Virol. 2021;93(1):336-50. https://doi.org/10.1002/jmv.26314
Flores-Silva FD, García-Grimshaw M, Valdés-Ferrer SI, Vigueras-Hernández AP, Domínguez-Moreno R, Tristán-Samaniego DP, et al. Neurologic manifestations in hospitalized patients with COVID-19 in Mexico City. PLoS One. 2021;16(4):e0247433. https://doi.org/10.1371/journal.pone.0247433
Bedock D, Lassen PB, Mathian A, Moreau P, Couffignal J, Ciangura C, et al. Prevalence and severity of malnutrition in hospitalized COVID-19 patients. Clin Nutr ESPEN. 2020; 40:214-9. https://doi.org/10.1016/j.clnesp.2020.09.018
Wierdsma NJ, Kruizenga HM, Konings LA, Krebbers D, Jorissen JR, Joosten MI, et al. Poor nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission. Clin Nutr ESPEN. 2021; 43:369-76. https://doi.org/10.1016/j.clnesp.2021.03.021
Sikaroudi MK, Zonooz SR, Ebrahimi Z, Jebraili H, Farsi F, Talebi A, et al. Assessment of anorexia and weight loss during the infection and recovery period of patients with coronavirus disease 2019 (COVID-19). Clin Nutr Open Sci. 2021;40:102-10. https://doi.org/10.1016/j.nutos.2021.11.001
Ye Q, Wang B, Zhang T, Xu J, Shang S. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. Am J Physiol Gastrointest Liver Physiol. 2020;319(2):G245-52. https://doi.org/10.1152/ajpgi.00148.2020
Vaillant MF, Agier L, Martineau C, Philipponneau M, Romand D, Masdoua V, et al. Food intake and weight loss of surviving inpatients in the course of COVID-19 infection: A longitudinal study of the multicenter NutriCoviD30 cohort. Nutrition. 2022; 93:111433. https://doi.org/10.1016/j.nut.2021.111433
Tsuchiya H. Oral Symptoms Associated with COVID-19 and Their Pathogenic Mechanisms: A Literature Review. Dent J (Basel). 2021;9(3):32. https://doi.org/10.3390/dj9030032
Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. https://doi.org/10.1038/s41368-020-0074-x
Sato T, Ueha R, Goto T, Yamauchi A, Kondo K, Yamasoba T. Expression of ACE2 and TMPRSS2 Proteins in the Upper and Lower Aerodigestive Tracts of Rats: Implications on COVID 19 Infections. Laryngoscope. 2021;131(3):E932-39. https://doi.org/10.1002/lary.29132
Wang Z, Zhou J, Marshall B, Rekaya R, Ye K, Liu HX. SARS-CoV-2 Receptor ACE2 is enriched in a subpopulation of mouse tongue epithelial cells in nongustatory papillae but not in taste buds or embryonic oral epithelium. ACS Pharmacol Transl Sci. 2020;3(4):749-58. https://doi.org/10.1021/acsptsci.0c00062
Sakaguchi W, Kubota N, Shimizu T, Saruta J, Fuchida S, Kawata A, et al. Existence of SARS-CoV-2 entry molecules in the oral cavity. Int J Mol Sci. 2020;21(17):6000. https://doi.org/10.3390/ijms21176000
Vaira LA, Salzano G, Fois AG, Piombino P, De Riu G. Potential pathogenesis of ageusia and anosmia in COVID-19 patients. Int Forum Allergy Rhinol. 2020;10(9):1103-4. https://doi.org/10.1002/alr.22593
Finsterer J, Stollberger C. Causes of hypogeusia/hyposmia in SARS-CoV2 infected patients. J Med Virol. 2020;92(10):1793-4. https://doi.org/10.1002/jmv.25903
Milanetti E, Miotto M, Di Rienzo L, Nagaraj M, Monti M, Golbek TW,et al. In-Silico Evidence for a Two Receptor Based Strategy of SARS-CoV-2. Front Mol Biosci. 2021;8:690655. https://doi.org/10.3389/fmolb.2021.690655
Mariz BALA, Brandão TB, Ribeiro ACP, Lopes MA, Santos-Silva AR. New Insights for the Pathogenesis of COVID-19-Related Dysgeusia. J Dent Res. 2020;99(10):1206. https://doi.org/10.1177/0022034520936638
Dos Santos JA, Normando AGC, Da Silva RLC, Acevedo AC, Canto GL, Sugaya N, et al. Oral Manifestations in Patients with COVID-19: A Living Systematic Review. J Dent Res. 2021;100(2):141-54. https://doi.org/10.1177/0022034520957289
Antwi J, Appiah B, Oluwakuse B, Abu BAZ. The Nutrition-COVID-19 Interplay: a Review. Curr Nutr Rep. 2021;10(4):364-74. https://doi.org/10.1007/s13668-021-00380-2
Alves TCHS, Guimarães RS, Souza SF, Brandão NA, Daltro CHDC, Conceição-Machado MEP, et al. Influence of nutritional assistance on mortality by COVID-19 in critically ill patients. Clin Nutr ESPEN. 2021; 44:469-71. https://doi.org/10.1016/j.clnesp.2021.05.016
Pironi L, Sasdelli AS, Ravaioli F, Baracco B, Battaiola C, Bocedi G, et al. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin Nutr. 2021;40(3):1330-7. https://doi.org/10.1016/j.clnu.2020.08.021
Nakamura K, Liu K, Katsukawa H, Nydahl P, Ely EW, Kudchadkar SR, et al. Nutrition therapy in the intensive care unit during the COVID-19 pandemic: Findings from the ISIIC point prevalence study. Clin Nutr. 2021;S0261-5614(21)00450-7. https://doi.org/10.1016/j.clnu.2021.09.033
Cereda E, Guzzardella A, Klersy C, Belliato M, Pellegrini A, Sciutti F, et al. Early caloric deficit is associated with a higher risk of death in invasive ventilated COVID-19 patients. Clin Nutr. 2021;S0261-5614(21)00094-7. https://doi.org/10.1016/j.clnu.2021.02.020
Miguélez M, Velasco C, Camblor M, Cedeño J, Serrano C, Bretón I, et al. Nutritional management and clinical outcome of critically ill patients with COVID-19: A retrospective study in a tertiary hospital. Clin Nutr. 2021;S0261-5614(21)00499-4. https://doi.org/10.1016/j.clnu.2021.10.020
Alencar ES, Muniz LSDS, Holanda JLG, Oliveira BDD, Carvalho MCF, Leitão AMM, et al. Enteral nutritional support for patients hospitalized with COVID-19: Results from the first wave in a public hospital. Nutrition. 2022;94:111512. https://doi.org/10.1016/j.nut.2021.111512
Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39(6):1631-8. https://doi.org/10.1016/j.clnu.2020.03.022
Stachowska E, Folwarski M, Jamioł-Milc D, Maciejewska D, Skonieczna-Żydecka K. Nutritional Support in Coronavirus 2019 Disease. Medicina (Kaunas). 2020;56(6):289. https://doi.org/10.3390/medicina56060289
Laviano A, Koverech A, Zanetti M. Nutrition support in the time of SARS-CoV-2 (COVID-19). Nutrition. 2020;74:110834. https://doi.org/10.1016/j.nut.2020.110834