The role of iron and ferritin in pathophysiology and as a laboratory marker in COVID-19
Main Article Content
Abstract
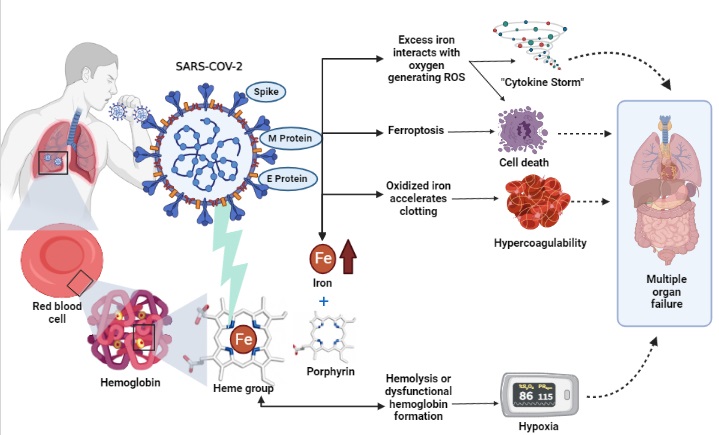
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) emerged in China exponentially and is recognized as a multisystem disease that gradually elevates markers associated with iron metabolism as the infection becomes more intense, becoming a critical factor in the investigation of prognosis. We review the latest scientific findings on the behavior of iron and ferritin in pathophysiology and as laboratory markers in COVID-19 (Coronavirus Disease 2019).The findings showed that iron and ferritin play a key role in the pathogenesis of COVID-19, contributing to the worsening of the disease. Therefore, iron dysmetabolism, marked by hyperferritinemia, is associated with inflammatory states in SARS-CoV-2 infection, and ferritin measurement has been shown to be a useful laboratory marker with a clinical and discriminatory potential to define the severity and mortality during COVID-19.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Xu J, Ma XP, Bai L, Wang M, Deng W, Ning N. A systematic review of etiology, epidemiology, clinical manifestations, image findings, and medication of 2019 Corona Virus Disease-19 in Wuhan, China. Medicine. 2020;99(42):e22688. https://doi.org/10.1097/MD.0000000000022688 DOI: https://doi.org/10.1097/MD.0000000000022688
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33. https://doi.org/10.1056/NEJMoa2001017 DOI: https://doi.org/10.1056/NEJMoa2001017
Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020;10(2):1271. https://doi.org/10.4081/cp.2020.1271 DOI: https://doi.org/10.4081/cp.2020.1271
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-13. https://doi.org/10.1016/S0140-6736(20)30211-7 DOI: https://doi.org/10.1016/S0140-6736(20)30211-7
Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020;57(6):389-99. https://doi.org/10.1080/10408363.2020.1770685 DOI: https://doi.org/10.1080/10408363.2020.1770685
Lv Y, Chen L, Liang X, Liu X, Gao M, Wang Q, et al. Association between iron status and the risk of adverse outcomes in COVID-19. Clin Nutr. 2021;40(5):3462-9. https://doi.org/10.1016/j.clnu.2020.11.033 DOI: https://doi.org/10.1016/j.clnu.2020.11.033
Ganz T, Nemeth E. Iron homeostasis in host defence and inflammation. Nat Rev Immunol. 2015;15(8):500-10. https://doi.org/10.1038/nri3863 DOI: https://doi.org/10.1038/nri3863
Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29(9):401-9. https://doi.org/10.1093/intimm/dxx031 DOI: https://doi.org/10.1093/intimm/dxx031
Coffey R, Ganz T. Iron homeostasis: An anthropocentric perspective. J Biol Chem. 2017;292(31):12727-34. https://doi.org/10.1074/jbc.R117.781823 DOI: https://doi.org/10.1074/jbc.R117.781823
Girelli D, Marchi G, Busti F, Vianello A. Iron metabolism in infections: Focus on COVID-19. Semin Hematol. 2021;58(3):182-7. https://doi.org/10.1053/j.seminhematol.2021.07.001 DOI: https://doi.org/10.1053/j.seminhematol.2021.07.001
Perricone C, Bartoloni E, Bursi R, Cafaro G, Guidelli GM, Shoenfeld Y, et al. COVID-19 as part of the hyperferritinemic syndromes: the role of iron depletion therapy. Immunol Res. 2020;68(4):213-24. https://doi.org/10.1007/s12026-020-09145-5 DOI: https://doi.org/10.1007/s12026-020-09145-5
Ganz T. Iron and infection. Int J Hematol. 2018;107(1):7-15. https://doi.org/10.1007/s12185-017-2366-2 DOI: https://doi.org/10.1007/s12185-017-2366-2
Wessling-Resnick M. Iron homeostasis and the inflammatory response. Annu Rev Nutr. 2010;30:105-22. https://doi.org/10.1146/annurev.nutr.012809.104804 DOI: https://doi.org/10.1146/annurev.nutr.012809.104804
Camaschella C. Iron deficiency: new insights into diagnosis and treatment. Hematology Am Soc Hematol Educ Program. 2015;2015:8-13. https://doi.org/10.1182/asheducation-2015.1.8 DOI: https://doi.org/10.1182/asheducation-2015.1.8
Wang CY, Babitt JL. Hepcidin regulation in the anemia of inflammation. Curr Opin Hematol. 2016;23(3):189-97. https://doi.org/10.1097/MOH.0000000000000236 DOI: https://doi.org/10.1097/MOH.0000000000000236
Daher R, Manceau H, Karim Z. Iron metabolism and the role of the iron-regulating hormone hepcidin in health and disease. Presse Med. 2017;46(12 Pt 2):e272-e8. https://doi.org/10.1016/j.lpm.2017.10.006 DOI: https://doi.org/10.1016/j.lpm.2017.10.006
Polak SB, Van Gool IC, Cohen D, von der Thüsen JH, van Paassen J. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod Pathol. 2020;33(11):2128-38. https://doi.org/10.1038/s41379-020-0603-3 DOI: https://doi.org/10.1038/s41379-020-0603-3
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3 DOI: https://doi.org/10.1016/S0140-6736(20)30566-3
Shang J, Ye G, Shi K, Wan Y, Luo C, Aihara H, et al. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020;581(7807):221-4. https://doi.org/10.1038/s41586-020-2179-y DOI: https://doi.org/10.1038/s41586-020-2179-y
Cheng H, Wang Y, Wang GQ. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J Med Virol. 2020;92(7):726-30. https://doi.org/10.1002/jmv.25785 DOI: https://doi.org/10.1002/jmv.25785
Murray E, Tomaszewski M, Guzik TJ. Binding of SARS-CoV-2 and angiotensin-converting enzyme 2: clinical implications. Cardiovasc Res. 2020;116(7):e87-e9. https://doi.org/10.1093/cvr/cvaa096 DOI: https://doi.org/10.1093/cvr/cvaa096
Imai Y, Kuba K, Penninger JM. The discovery of angiotensin-converting enzyme 2 and its role in acute lung injury in mice. Exp Physiol. 2008;93(5):543-8. https://doi.org/10.1113/expphysiol.2007.040048 DOI: https://doi.org/10.1113/expphysiol.2007.040048
Habib HM, Ibrahim S, Zaim A, Ibrahim WH. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed Pharmacother. 2021;136:111228. https://doi.org/10.1016/j.biopha.2021.111228 DOI: https://doi.org/10.1016/j.biopha.2021.111228
Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92(4):424-32. https://doi.org/10.1002/jmv.25685 DOI: https://doi.org/10.1002/jmv.25685
Ye Q, Wang B, Mao J. The pathogenesis and treatment of the 'Cytokine Storm' in COVID-19. J Infec. 2020;80(6):607-13. https://doi.org/10.1016/j.jinf.2020.03.037 DOI: https://doi.org/10.1016/j.jinf.2020.03.037
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-4. https://doi.org/10.1016/S0140-6736(20)30628-0 DOI: https://doi.org/10.1016/S0140-6736(20)30628-0
Liu W, Li HJCd. COVID-19: Attacks the 1-beta chain of hemoglobin and captures the porphyrin to inhibit human heme metabolism. ChemRxiv. 2022 (Preprint). https://doi.org/10.26434/chemrxiv-2021-dtpv3-v11 DOI: https://doi.org/10.26434/chemrxiv-2021-dtpv3-v11
Kell DB, Pretorius E. Serum ferritin is an important inflammatory disease marker, as it is mainly a leakage product from damaged cells. Metallomics. 2014;6(4):748-73. https://doi.org/10.1039/C3MT00347G DOI: https://doi.org/10.1039/C3MT00347G
Wenzhong L, Hualan L. COVID-19: captures iron and generates reactive oxygen species to damage the human immune system. Autoimmunity. 2021;54(4):213-24. https://doi.org/10.1080/08916934.2021.1913581 DOI: https://doi.org/10.26434/chemrxiv.13301372
Sun Y, Chen P, Zhai B, Zhang M, Xiang Y, Fang J, et al. The emerging role of ferroptosis in inflammation. Biomed Pharmacother. 2020;127:110108. https://doi.org/10.1016/j.biopha.2020.110108 DOI: https://doi.org/10.1016/j.biopha.2020.110108
Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and Ageusia: Common Findings in COVID-19 Patients. Laryngoscope. 2020;130(7):1787. https://doi.org/10.1002/lary.28692 DOI: https://doi.org/10.1002/lary.28692
Temraz S, Santini V, Musallam K, Taher A. Iron overload and chelation therapy in myelodysplastic syndromes. Crit Rev Oncol Hematol. 2014;91(1):64-73. https://doi.org/10.1016/j.critrevonc.2014.01.006 DOI: https://doi.org/10.1016/j.critrevonc.2014.01.006
Wang W, Knovich MA, Coffman LG, Torti FM, Torti SV. Serum ferritin: Past, present and future. Biochim Biophys Acta. 2010;1800(8):760-9. https://doi.org/10.1016/j.bbagen.2010.03.011 DOI: https://doi.org/10.1016/j.bbagen.2010.03.011
Suchdev PS, Williams AM, Mei Z, Flores-Ayala R, Pasricha SR, Rogers LM, et al. Assessment of iron status in settings of inflammation: challenges and potential approaches. Am J Clin Nutr. 2017;106(Suppl 6):1626s-33s. https://doi.org/10.3945/ajcn.117.155937 DOI: https://doi.org/10.3945/ajcn.117.155937
Ruscitti P, Giacomelli R. Ferritin and Severe COVID-19, from clinical observations to pathogenic implications and therapeutic perspectives. Isr Med Assoc J. 2020;22(8):516-8. PMId:33236586
Gómez-Pastora J, Weigand M, Kim J, Wu X, Strayer J, Palmer AF, et al. Hyperferritinemia in critically ill COVID-19 patients - Is ferritin the product of inflammation or a pathogenic mediator? Clin Chim Acta. 2020;509:249-51. https://doi.org/10.1016/j.cca.2020.06.033 DOI: https://doi.org/10.1016/j.cca.2020.06.033
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854-87. https://doi.org/10.1007/s00134-020-06022-5 DOI: https://doi.org/10.1007/s00134-020-06022-5
Banchini F, Cattaneo GM, Capelli P. Serum ferritin levels in inflammation: a retrospective comparative analysis between COVID-19 and emergency surgical non-COVID-19 patients. World J Emerg Surg. 2021;16(1):9. https://doi.org/10.1186/s13017-021-00354-3 DOI: https://doi.org/10.1186/s13017-021-00354-3
Bellmann-Weiler R, Lanser L, Barket R, Rangger L, Schapfl A, Schaber M, et al. Prevalence and predictive value of anemia and dysregulated iron homeostasis in patients with COVID-19 infection. J Clin Med. 2020;9(8):2429. https://doi.org/10.3390/jcm9082429 DOI: https://doi.org/10.3390/jcm9082429
Bolondi G, Russo E, Gamberini E, Circelli A, Meca MCC, Brogi E, et al. Iron metabolism and lymphocyte characterisation during Covid-19 infection in ICU patients: an observational cohort study. World J Emerg Surg. 2020;15(1):41. https://doi.org/10.1186/s13017-020-00323-2 DOI: https://doi.org/10.1186/s13017-020-00323-2
Dahan S, Segal G, Katz I, Hellou T, Tietel M, Bryk G, et al. Ferritin as a Marker of Severity in COVID-19 Patients: A Fatal Correlation. Isr Med Assoc J. 2020;22(8):494-500. PMId:33236582
Hippchen T, Altamura S, Muckenthaler MU, Merle U. Hypoferremia is associated with increased hospitalization and oxygen demand in COVID-19 patients. HemaSphere. 2020;4(6):e492. https://doi.org/10.1097/HS9.0000000000000492 DOI: https://doi.org/10.1097/HS9.0000000000000492
Sonnweber T, Boehm A, Sahanic S, Pizzini A, Aichner M, Sonnweber B, et al. Persisting alterations of iron homeostasis in COVID-19 are associated with non-resolving lung pathologies and poor patients' performance: a prospective observational cohort study. Respir Res. 2020;21(1):276. https://doi.org/10.1186/s12931-020-01546-2 DOI: https://doi.org/10.1186/s12931-020-01546-2
Tojo K, Sugawara Y, Oi Y, Ogawa F, Higurashi T, Yoshimura Y, et al. The U-shaped association of serum iron level with disease severity in adult hospitalized patients with COVID-19. Sci Rep. 2021;11(1):13431. https://doi.org/10.1038/s41598-021-92921-6 DOI: https://doi.org/10.1038/s41598-021-92921-6
Zhou C, Chen Y, Ji Y, He X, Xue D. Increased serum levels of hepcidin and ferritin are associated with severity of COVID-19. Med Sci Monit. 2020;26:e926178. https://doi.org/10.12659/MSM.926178 DOI: https://doi.org/10.12659/MSM.926178
Ahmed S, Ansar Ahmed Z, Siddiqui I, Haroon Rashid N, Mansoor M, Jafri L. Evaluation of serum ferritin for prediction of severity and mortality in COVID-19- A cross sectional study. Ann Med Surg. 2021;63:102163. https://doi.org/10.1016/j.amsu.2021.02.009 DOI: https://doi.org/10.1016/j.amsu.2021.02.009
Raman N, Kv P, Ashta KK, Vardhan V, Thareja S, J M, et al. Ferritin and hemoglobin as predictors of fatal outcome in COVID-19: two sides of the same coin. J Assoc Physicians India. 2021;69(8):11-2. PMId:34472812 DOI: https://doi.org/10.4103/jacp.jacp_44_21
Yağcı S, Serin E, Acicbe Ö, Zeren M, Odabaşı MS. The relationship between serum erythropoietin, hepcidin, and haptoglobin levels with disease severity and other biochemical values in patients with COVID-19. Int J Lab Hematol. 2021;43 Suppl 1(suppl 1):142-51. https://doi.org/10.1111/ijlh.13479 DOI: https://doi.org/10.1111/ijlh.13479
Colafrancesco S, Alessandri C, Conti F, Priori R. COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun rev. 2020;19(7):102573. https://doi.org/10.1016/j.autrev.2020.102573 DOI: https://doi.org/10.1016/j.autrev.2020.102573
Rosário C, Shoenfeld Y. The hyperferritinemic syndrome. Isr Med Assoc J. 2014;16(10):664-5. PMId:25438466