Osteometabolic changes in patients under antineoplastic treatment: scoping review
Main Article Content
Abstract
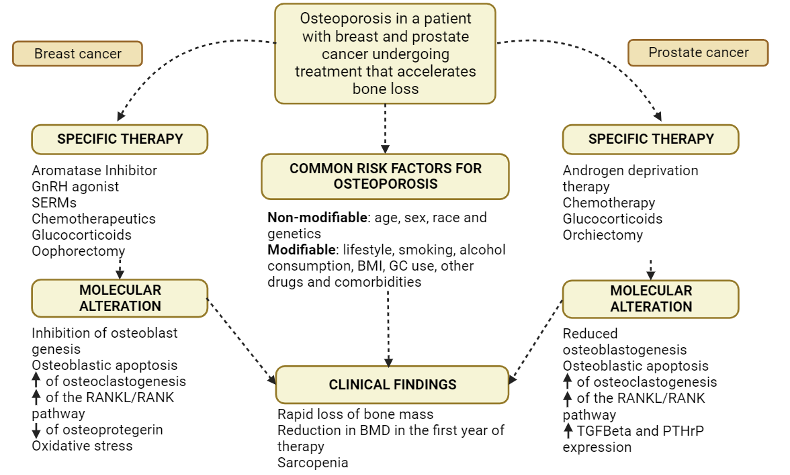
Objective: To summarize the main evidence regarding osteometabolic changes in patients undergoing antineoplastic treatment. Methods: This is a scoping review, following the methodology of the Joanna Briggs Institute, using PubMed/MedLine, Cochrane Library, LILACS, The British Library, and Google Scholar. This review is registered in the Open Science Framework. Results: Many antineoplastics affect bone architecture by reducing its density, such as selective estrogen receptor modulators, aromatase inhibitors, androgen deprivation therapy, and glucocorticoids. To avoid such outcomes, treatment and prevention can be achieved by calcium and vitamin D supplementation, physical exercise, use of bisphosphonates, denosumab, and selective estrogen receptor modulators. Conclusion: people at a higher risk of developing cancer also have a higher risk of osteopenia and osteoporosis when the process is already established and undergoing antineoplastic treatment because of the grouping of risk factors. The need for bone densitometry in patients undergoing cancer treatment to prevent and promote bone health in these patients is evident, in addition to more research with a high level of evidence to support such use.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Can Clin J. 2021;71(3):209-49. https://doi.org/10.3322/caac.21660 DOI: https://doi.org/10.3322/caac.21660
Bedatsova L, Drake MT. The skeletal impact of cancer therapies. Br J Clin Pharmacol. 2019;85(6):1161-8. https://doi.org/10.1111/bcp.13866 DOI: https://doi.org/10.1111/bcp.13866
Reuss-Borst M, Hartmann U, Scheede C, Weiß J. Prevalence of osteoporosis among cancer patients in Germany. Osteoporos Int. 2011;23(4):1437-44. https://doi.org/10.1007/s00198-011-1724-9 DOI: https://doi.org/10.1007/s00198-011-1724-9
Park SH, Knobf MT, Sutton KM. Etiology, assessment, and management of aromatase inhibitor-related musculoskeletal symptoms. Clin J Oncol Nurs. 2012;16(3):260-6. https://doi.org/10.1188/12.CJON.260-266 DOI: https://doi.org/10.1188/12.CJON.260-266
Van Poznak C, Somerfield MR, Barlow WE et al. Role of bone-modifying agents in metastatic breast cancer: an american society of clinical oncology-cancer care ontario focused guideline update. J Clin Oncol. 2017;35(35):3978-86. https://doi.org/10.1200/JCO.2017.75.4614 DOI: https://doi.org/10.1200/JCO.2017.75.4614
Rachner TD, Coleman R, Hadji P, Hofbauer LC. Bone health during endocrine therapy for cancer. Lancet Diabetes Amp Endocrinol. 2018;6(11):901-10. https://doi.org/10.1016/S2213-8587(18)30047-0 DOI: https://doi.org/10.1016/S2213-8587(18)30047-0
Morgan RL, Whaley P, Thayer KA, Schünemann HJ. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. 2018;121:1027-31. https://doi.org/10.1016/j.envint.2018.07.015 DOI: https://doi.org/10.1016/j.envint.2018.07.015
Melnyk BM, Ellen Fineout-Overholt E. Evidence-Based Practice in Nursing & Healthcare: A Guide to Best Practice (4th ed). LWW: Philadelphia, PA; 2018.
Lopes-Júnior LC, Bomfim E, Olson K, et al. Effectiveness of hospital clowns for symptom management in paediatrics: systematic review of randomised and non-randomised controlled trials. BMJ. 2020;371:m4290. https://doi.org/10.1136/bmj.m4290 DOI: https://doi.org/10.1136/bmj.m4290
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (Prisma-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467. https://doi.org/10.7326/M18-0850 DOI: https://doi.org/10.7326/M18-0850
Lopes-Júnior LC, Rosa MA, Lima RA. Psychological and psychiatric outcomes following PICU admission. Pediatr Crit Care Med. 2018;19(1):e58-67. https://doi.org/10.1097/PCC.0000000000001390 DOI: https://doi.org/10.1097/PCC.0000000000001390
Casemiro LK, Lopes-Júnior LC, Jardim FA, Sulino MC, de Lima RA. Telehealth in outpatient care for children and adolescents with chronic conditions during the COVID-19 pandemic: a scoping review protocol. PLoS One. 2022;17(6):e0269821 https://doi.org/10.1371/journal.pone.0269821 DOI: https://doi.org/10.1371/journal.pone.0269821
Law M. Guideline for Critical Review Form - Quantitative Studies. McMaster University Occupational Therapy Evidence-Based Practice Research Group; Canadá.1998. Available from: https://bit.ly/3EzQm0O DOI: https://doi.org/10.1177/000841749806500301
El Badri S, Salawu A, Brown JE. Bone health in men with prostate cancer: review article. Curr Osteoporos Rep. 2019;17(6):527-37. https://doi.org/10.1007/s11914-019-00536-8 DOI: https://doi.org/10.1007/s11914-019-00536-8
Liuhto N, Grönroos MH, Malila N, Madanat‐Harjuoja L, Matomäki J, Lähteenmäki P. Diseases of renal function and bone metabolism after treatment for early onset cancer: a registry‐based study. Int J Cancer. 2019;146(5):1324-32. https://doi.org/10.1002/ijc.32687 DOI: https://doi.org/10.1002/ijc.32687
Owen PJ, Daly RM, Livingston PM, Fraser SF. Lifestyle guidelines for managing adverse effects on bone health and body composition in men treated with androgen deprivation therapy for prostate cancer: an update. Prostate Cancer Prostatic Dis. 2017;20(2):137-45. https://doi.org/10.1038/pcan.2016.69 DOI: https://doi.org/10.1038/pcan.2016.69
Schyrr F, Wolfer A, Pasquier J, Nicoulaz AL, Lamy O, Naveiras O. Correlation study between osteoporosis and hematopoiesis in the context of adjuvant chemotherapy for breast cancer. Ann Hematol. 2017;97(2):309-17. https://doi.org/10.1007/s00277-017-3184-6
van Hellemond IEG, Smorenburg CH, Peer PGM, Swinkels ACP, Seynaeve CM, van der Sangen MJC, et al. Breast cancer outcome in relation to bone mineral density and bisphosphonate use: a sub-study of the DATA trial. Breast Cancer Res Treat. 2020;180(3):675-85. https://doi.org/10.1007/s10549-020-05567-9 DOI: https://doi.org/10.1007/s10549-020-05567-9
Seland M, Smeland KB, Bjøro T, Falk RS, Fosså SD, Gjesdal CG, et al. Bone mineral density is close to normal for age in long-term lymphoma survivors treated with high-dose therapy with autologous stem cell transplantation. Acta Oncol. 2017;56(4):590-8. https://doi.org/10.1080/0284186X.2016.1267870 DOI: https://doi.org/10.1080/0284186X.2016.1267870
Sestak I, Blake GM, Patel R, Coleman RE, Cuzick J, Eastell R. Comparison of risedronate versus placebo in preventing anastrozole-induced bone loss in women at high risk of developing breast cancer with osteopenia. Bone. 2019;124:83-8. https://doi.org/10.1016/j.bone.2019.04.016 DOI: https://doi.org/10.1016/j.bone.2019.04.016
Castañeda S, Casas A, González-Del-Alba A, Martínez-Díaz-Guerra G, Nogués X, Ojeda Thies C, et al. Bone loss induced by cancer treatments in breast and prostate cancer patients. Clin Transl Oncol. 2022;24(11):2090-106. https://doi.org/10.1007/s12094-022-02872-1 DOI: https://doi.org/10.1007/s12094-022-02872-1
Majithia N, Atherton PJ, Lafky JM, Wagner-Johnston N, Olson J, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2015;24(3):1219-26. https://doi.org/10.1007/s00520-015-2915-2 DOI: https://doi.org/10.1007/s00520-015-2915-2
Livi L, Scotti V, Desideri I, Saieva C, Cecchini S, Francolini G, et al. Phase 2 placebo-controlled, single-blind trial to evaluate the impact of oral ibandronate on bone mineral density in osteopenic breast cancer patients receiving adjuvant aromatase inhibitors: 5-year results of the single-centre BONADIUV trial. Eur J Cancer. 2019;108:100-110. https://doi.org/10.1016/j.ejca.2018.12.005 DOI: https://doi.org/10.1016/j.ejca.2018.12.005
Harvey NC, Glüer CC, Binkley N et al. Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone. 2015;78:216-24. https://doi.org/10.1016/j.bone.2015.05.016 DOI: https://doi.org/10.1016/j.bone.2015.05.016
Lane NE. Glucocorticoid-Induced osteoporosis: new insights into the pathophysiology and treatments. Curr Osteoporos Rep. 2019;17(1):1-7. https://doi.org/10.1007/s11914-019-00498-x DOI: https://doi.org/10.1007/s11914-019-00498-x
Smith MR, Fallon MA, Lee H, Finkelstein JS. Raloxifene to prevent gonadotropin-releasing hormone agonist-induced bone loss in men with prostate cancer: a randomized controlled trial. J Clin Endocrinol Amp Metab. 2004;89(8):3841-6. https://doi.org/10.1210/jc.2003-032058 DOI: https://doi.org/10.1210/jc.2003-032058
Gao Q, López-Knowles E, Cheang MC et al. Impact of aromatase inhibitor treatment on global gene expression and its association with antiproliferative response in ER+ breast cancer in postmenopausal patients. Breast Cancer Res. 2019;22(1):2. https://doi.org/10.1186/s13058-019-1223-z DOI: https://doi.org/10.1186/s13058-019-1223-z
Schyrr F, Wolfer A, Pasquier J, Nicoulaz AL, Lamy O, Naveiras O. Correlation study between osteoporosis and hematopoiesis in the context of adjuvant chemotherapy for breast cancer. Ann Hematol. 2017;97(2):309-17. https://doi.org/10.1007/s00277-017-3184-6 DOI: https://doi.org/10.1007/s00277-017-3184-6
Paterson AH, Anderson SJ, Lembersky BC et al. Oral clodronate for adjuvant treatment of operable breast cancer (National Surgical Adjuvant Breast and Bowel Project protocol B-34): a multicentre, placebo-controlled, randomised trial. Lancet Oncol. 2012;13(7):734-42. https://doi.org/10.1016/S1470-2045(12)70226-7 DOI: https://doi.org/10.1016/S1470-2045(12)70226-7
EBCTCG (Early Breast Cancer Trialists' Collaborative Group). Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127-35. https://doi.org/10.1016/S0140-6736(14)60488-8 DOI: https://doi.org/10.1016/S0140-6736(14)60488-8
Denham JW, Joseph D, Lamb DS, Spry NA, Duchesne G, Matthews J, et al. Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): 10-year results from a randomised, phase 3, factorial trial. Lancet Oncol. 2019;20(2):267-81. https://doi.org/10.1016/S1470-2045(18)30757-5 DOI: https://doi.org/10.1016/S1470-2045(18)30757-5
Clarke BL. Denosumab in men receiving androgen-deprivation therapy for prostate cancer. Yearb Med. 2010;2010:487-9. https://doi.org/10.1016/S0084-3873(10)79797-2 DOI: https://doi.org/10.1016/S0084-3873(10)79797-2