Association between weight loss and reduced use of antihypertensive, hypoglycemic, psychotropic, and lipid-lowering drugs in patients undergoing bariatric surgery
Main Article Content
Abstract
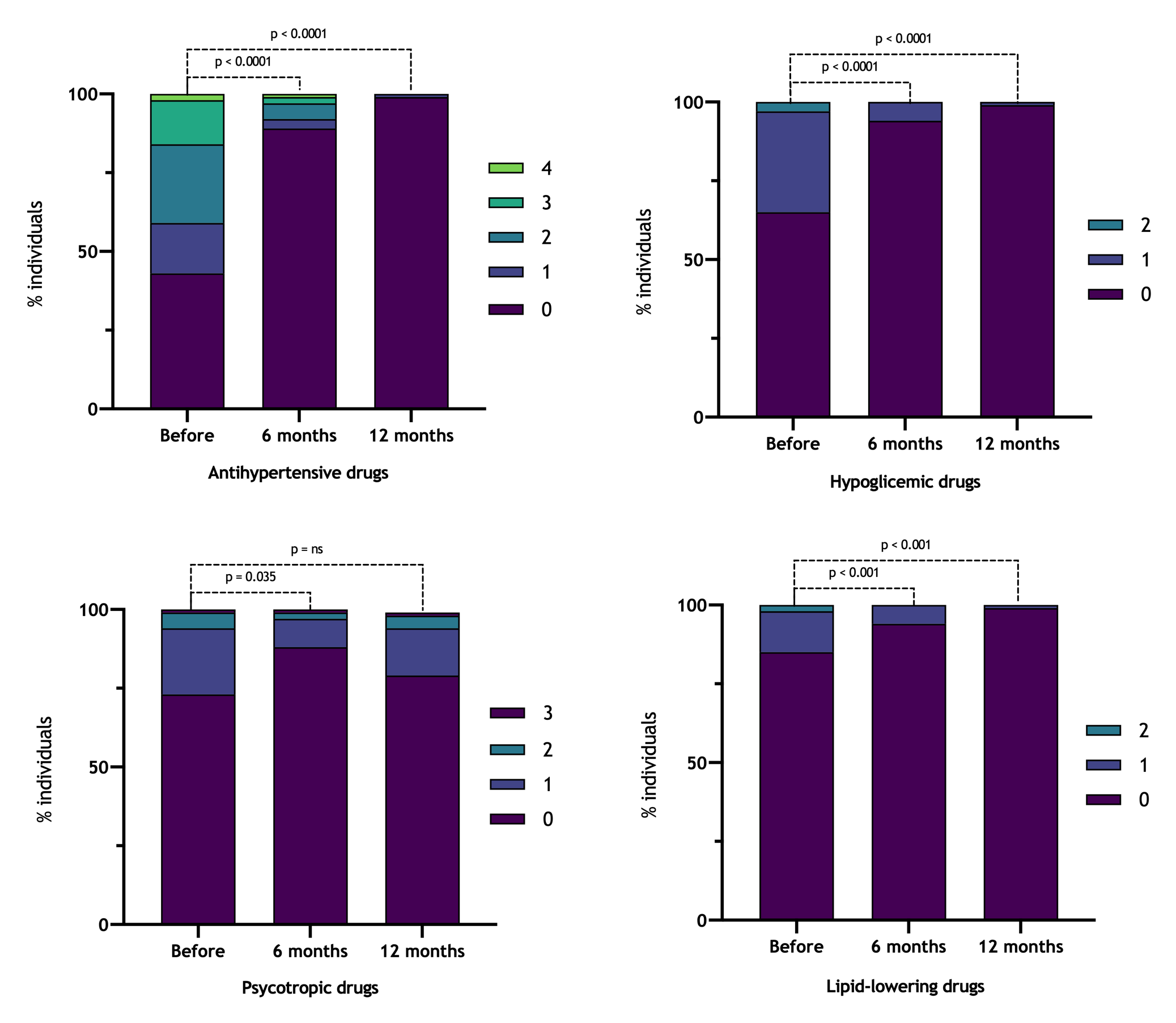
Objectives: To analyze whether the weight reduction observed in bariatric surgery (Roux-en-Y gastric bypass; BGYR) is accompanied by a reduction in the use of antihypertensive, hypoglycemic, antilipidemic, and psychotropic drugs after 6 and 12 months. Methods: Longitudinal, retrospective study of 100 adult patients undergoing RYGB from May 2015 to January 2019, by laparotomy or laparoscopy. Data on age, body mass index (BMI), and the number of drugs used were recorded 6 and 12 months after surgery. Results: The mean age was 39.7 ± 9.7 years, and the majority were female (n = 78). The mean preoperative BMI was 43.7 ± 5.1 kg/m2, and the mean reduction in BMI after 6 months was 12.1 kg/m2 and 14.9 kg/m2 after 12 months. The reduction in antihypertensive drugs was 65.2% after 6 months and 96% after 12 months. The reduction in 6 months of hypoglycemic agents was 84.3%, and in 12 months, 98.3%. The average reduction in antidyslipidemic drugs was 86.7% in 6 months, and there was no record of using this medication after 12 months. Psychotropics showed a temporary reduction in use after 6 months with a return to levels close to the baseline after 1 year.There was no correlation between the variation in BMI and the use of drugs. Conclusions: there was a significant reduction in the use of drugs after 6 and 12 m, except for psychotropic drugs. The reduction in the use of drugs was not correlated with a reduction in BMI.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Cohen JB. Hypertension in obesity and the impact of weight loss. Curr Cardiol Rep. 2017;19(10):98. https://doi.org/10.1007/s11886-017-0912-4 PMid:28840500 PMCid:PMC5606235 DOI: https://doi.org/10.1007/s11886-017-0912-4
Costa ACC, Ivo ML, Cantero WB, Tognini JRF. Obesidade em pacientes candidatos a cirurgia bariátrica. Acta Paul Enferm. 2009;22(1):55-9. https://doi.org/10.1590/S0103-21002009000100009 DOI: https://doi.org/10.1590/S0103-21002009000100009
Benraouane F, Litwin SE. Reductions in cardiovascular risk after bariatric surgery. Curr Opin Cardiol. 2011;26(6):555-61. https://doi.org/10.1097/HCO.0b013e32834b7fc4 PMid:21934498 PMCid:PMC4070434 DOI: https://doi.org/10.1097/HCO.0b013e32834b7fc4
Singh P, Subramanian A, Adderley N, Gokhale K, Singhal R, Bellary S, et al. Impact of bariatric surgery on cardiovascular outcomes and mortality: a population‐based cohort study. Brit J Surg. 2020;107(4):432-42. https://doi.org/10.1002/bjs.11433 PMid:31965568 DOI: https://doi.org/10.1002/bjs.11433
Pontiroli AE, Ceriani V, Tagliabue E. Compared with controls, bariatric surgery prevents long-term mortality in persons with obesity only above median age of cohorts: a systematic review and meta-analysis. Obes Surg. 2020;30(7):2487-96. https://doi.org/10.1007/s11695-020-04530-3 PMid:32152843 DOI: https://doi.org/10.1007/s11695-020-04530-3
Hussain S, Khan MS, Jamali MC, Siddiqui AN, Gupta G, Hussain MS, et al. Impact of bariatric surgery in reducing macrovascular complications in severely obese T2DM patients. Obes Surg. 2021;1-8. [Epub ahead of print] https://doi.org/10.1007/s11695-020-05155-2 DOI: https://doi.org/10.1007/s11695-020-05155-2
Jabbour G, Salman A. Bariatric Surgery in adults with obesity: the impact on performance, metabolism, and health indices. Obes Surg. 2021;1-23. [Epub ahead of print] https://doi.org/10.1007/s11695-020-05182-z PMid:33454846 DOI: https://doi.org/10.1007/s11695-020-05182-z
English WJ, Spann MD, Aher CV, Williams DB. Cardiovascular risk reduction following metabolic and bariatric surgery. Ann Transl Medicine. 2020;8(S1):S12. https://doi.org/10.21037/atm.2020.01.88 PMid:32309416 PMCid:PMC7154333 DOI: https://doi.org/10.21037/atm.2020.01.88
Schiavon CA, Bersch-Ferreira AC, Santucci EV, Oliveira JD, Torreglosa CR, Bueno PT, et al. Effects of bariatric surgery in obese patients with hypertension. Circulation. 2018;137(11):1132-42. https://doi.org/10.1161/CIRCULATIONAHA.117.032130 PMid:29133606 PMCid:PMC5865494 DOI: https://doi.org/10.1161/CIRCULATIONAHA.117.032130
Rubino F, R'bibo SL, Genio F del, Mazumdar M, McGraw TE. Metabolic surgery: the role of the gastrointestinal tract in diabetes mellitus. Nat Rev Endocrinol. 2010;6(2):102-9. https://doi.org/10.1038/nrendo.2009.268 PMid:20098450 PMCid:PMC2999518 DOI: https://doi.org/10.1038/nrendo.2009.268
Elliott JP, Gray EL, Yu J, Kalarchian MA. Medication use among patients prior to bariatric surgery. Bariatr Surg Pract P. 2015;10(3):105-9. https://doi.org/10.1089/bari.2015.0006 PMid:26421247 PMCid:PMC4575522 DOI: https://doi.org/10.1089/bari.2015.0006
Segal JB, Clark JM, Shore AD, Dominici F, Magnuson T, Richards TM, et al. Prompt reduction in use of medications for comorbid conditions after bariatric surgery. Obes Surg. 2009;19(12):1646-56. https://doi.org/10.1007/s11695-009-9960-1 PMid:19763709 DOI: https://doi.org/10.1007/s11695-009-9960-1
Backes CF, Lopes E, Tetelbom A, Heineck I. Medication and nutritional supplement use before and after bariatric surgery. Sao Paulo Med J. 2016;134(6):491-500. https://doi.org/10.1590/1516-3180.2015.0241030516 PMid:27812597 DOI: https://doi.org/10.1590/1516-3180.2015.0241030516
Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-91. https://doi.org/10.3758/BF03193146 PMid:17695343 DOI: https://doi.org/10.3758/BF03193146
Noria S, Grantcharov T. Biological effects of bariatric surgery on obesity-related comorbidities. Can J Surg. 2013;56(1):47-57. https://doi.org/10.1503/cjs.036111 PMid:23351555 PMCid:PMC3569476 DOI: https://doi.org/10.1503/cjs.036111
Puzziferri N, Roshek TB, Mayo HG, Gallagher R, Belle SH, Livingston EH. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312(9):934-42. https://doi.org/10.1001/jama.2014.10706 PMid:25182102 PMCid:PMC4409000 DOI: https://doi.org/10.1001/jama.2014.10706
Nguyen NT, Ho HS, Mayer KL, Palmer L, Wolfe BM. Laparoscopic Roux-en-Y gastric bypass for morbid obesity. J Soc Laparoendosc Surg Soc Laparoendosc Surg. 1999;3(3):193-6.
Chaim EA, Ramos AC, Cazzo E. Mini-gastric bypass: description of the technique and preliminary results. Arq Bras Cir Dig. 2017;30(4):264-6. https://doi.org/10.1590/0102-6720201700040009 PMid:29340551 PMCid:PMC5793145 DOI: https://doi.org/10.1590/0102-6720201700040009
Mingrone G, Panunzi S, Gaetano AD, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. New Engl J Medicine. 2012;366(17):1577-85. https://doi.org/10.1056/NEJMoa1200111 PMid:22449317 DOI: https://doi.org/10.1056/NEJMoa1200111
Docherty NG, Roux CW. Improvements in the metabolic milieu following Roux‐en‐Y gastric bypass and the arrest of diabetic kidney disease. Exp Physiol. 2014;99(9):1146-53. https://doi.org/10.1113/expphysiol.2014.078790 PMid:25085842 DOI: https://doi.org/10.1113/expphysiol.2014.078790
Shah M, Pham A, Gershuni V, Mundi MS. Curing diabetes through bariatric surgery: evolution of our understanding. Curr Surg Reports. 2018;6(7):11. https://doi.org/10.1007/s40137-018-0209-6 DOI: https://doi.org/10.1007/s40137-018-0209-6
Affinati AH, Esfandiari NH, Oral EA, Kraftson AT. Bariatric surgery in the treatment of type 2 diabetes. Curr Diabetes Rep. 2019;19(12):156. https://doi.org/10.1007/s11892-019-1269-4 PMid:31802258 PMCid:PMC7522929 DOI: https://doi.org/10.1007/s11892-019-1269-4
Monteforte MJ, Turkelson CM. Bariatric surgery for morbid obesity. Obes Surg. 2000;10(5):391-401. https://doi.org/10.1381/096089200321594246 PMid:11054242 DOI: https://doi.org/10.1381/096089200321594246
Novais PFS, Junior IR, Leite CVS, Oliveira MRM. Evolução e classificação do peso corporal em relação aos resultados da cirurgia bariátrica: derivação gástrica em Y de Roux. Arq Bras Endocrinol Metab. 2010;54(3):303-10. https://doi.org/10.1590/S0004-27302010000300009 PMid:20520961 DOI: https://doi.org/10.1590/S0004-27302010000300009
Yska JP, Meer DH van der, Dreijer AR, Eilander W, Apers JA, Emous M, et al. Influence of bariatric surgery on the use of medication. Eur J Clin Pharmacol. 2016;72(2):203-9. https://doi.org/10.1007/s00228-015-1971-3 PMid:26525890 DOI: https://doi.org/10.1007/s00228-015-1971-3
Laar AW van de, Brauw LM de, Meesters EW. Relationships between type 2 diabetes remission after gastric bypass and different weight loss metrics: arguments against excess weight loss in metabolic surgery. Surg Obes Relat Dis. 2016;12(2):274-82. https://doi.org/10.1016/j.soard.2015.07.005 PMid:26476492 DOI: https://doi.org/10.1016/j.soard.2015.07.005
Yska JP, Linde S van der, Tapper VV, Apers JA, Emous M, Totté ER, et al. Influence of bariatric surgery on the use and pharmacokinetics of some major drug classes. Obes Surg. 2013;23(6):819-25. https://doi.org/10.1007/s11695-013-0882-6 PMid:23430479 DOI: https://doi.org/10.1007/s11695-013-0882-6
Cunningham JL, Merrell CC, Sarr M, Somers KJ, McAlpine D, Reese M, et al. Investigation of antidepressant medication usage after bariatric surgery. Obes Surg. 2012;22(4):530-5. https://doi.org/10.1007/s11695-011-0517-8 PMid:21901283 DOI: https://doi.org/10.1007/s11695-011-0517-8
Gill H, Kang S, Lee Y, Rosenblat JD, Brietzke E, Zuckerman H, et al. The Long-term effect of bariatric surgery on depression and anxiety. J Affect Disorders. 2018;246:886-94. https://doi.org/10.1016/j.jad.2018.12.113 PMid:30795495 DOI: https://doi.org/10.1016/j.jad.2018.12.113
Makary MA, Clark JM, Clarke JM, Shore AD, Magnuson TH, Richards T, et al. Medication utilization and annual health care costs in patients with type 2 diabetes mellitus before and after bariatric surgery. Arch Surg. 2010;145(8):726-31. https://doi.org/10.1001/archsurg.2010.150 PMid:20713923 DOI: https://doi.org/10.1001/archsurg.2010.150
Larsen AT, Højgaard B, Ibsen R, Kjellberg J. The socio-economic impact of bariatric surgery. Obes Surg. 2018;28(2):338-48. https://doi.org/10.1007/s11695-017-2834-z PMid:28735376 DOI: https://doi.org/10.1007/s11695-017-2834-z
Weiner JP, Goodwin SM, Chang H-Y, Bolen SD, Richards TM, Johns RA, et al. Impact of bariatric surgery on health care costs of obese persons: a 6-year follow-up of surgical and comparison cohorts using health plan data. JAMA Surg. 2013;148(6):555-61. https://doi.org/10.1001/jamasurg.2013.1504 PMid:23426865 DOI: https://doi.org/10.1001/jamasurg.2013.1504
Wu T, Wong SKH, Law BTT, Grieve E, Wu O, Tong DKH, et al. Bariatric surgery is expensive but improves co‐morbidity: 5‐year assessment of patients with obesity and type 2 diabetes. Brit J Surg. 2020; [Epub ahead of print]. https://doi.org/10.1002/bjs.11970 PMid: 32990329