Analysis of requests for reservation of blood concentrates in patients referred to urgent surgeries in a teaching hospital
Main Article Content
Abstract
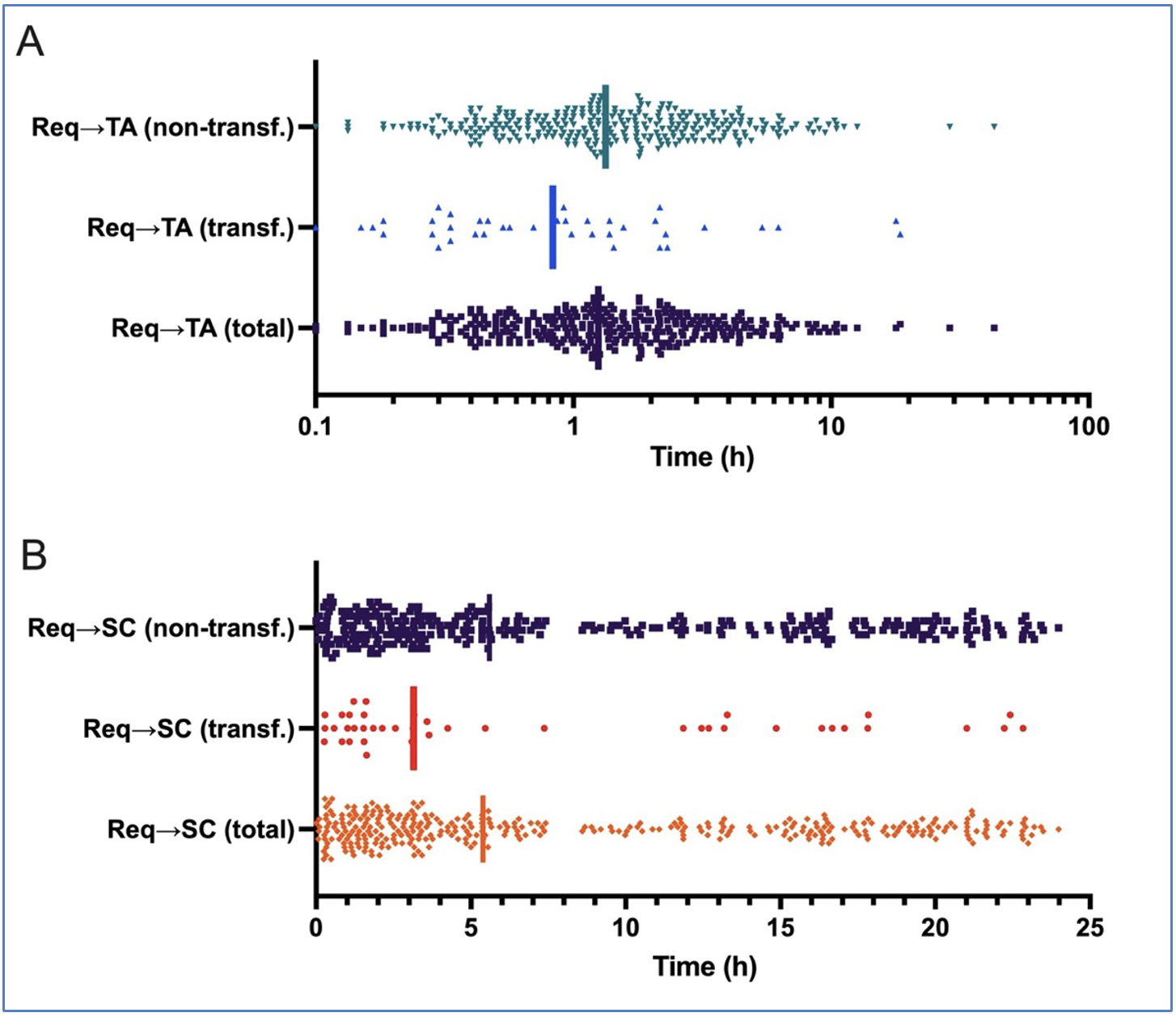
Introduction: The rates of request and use of blood concentrates are still poorly reported in the literature. This study aimed to analyze the rates of requests for blood concentrates and their use in patients undergoing emergency surgery in a teaching hospital. Methods: A retrospective, quantitative and descriptive study was conducted in 359 medical records of patients in urgent surgery scheduled with a request for a reserve of blood concentrate. The ratios between crossmatched and transfused units (C/T), transfusion index (TI), and probability (TP) were calculated, and the times between request and delivery at the transfusion agency (TA) and patient admission to the surgical center (SC). Results: The mean age was 58.5 ± 22.2 years, with the majority being male (53.1%). There was an average of 27.5 monthly requests (min 12, max 44). Ninety-seven units of blood concentrates were transfused into 44 patients (C/T ratio 7.59; TI 0.27; TP 12.3%). Only seven patients had their requests made after admission to the OR. The median time between the request and arrival at the TA was 1h15min, while that between the request and the patient's arrival at the SC was 5h23min. There was greater transfusion in major surgery (major 37, 14.8% vs. medium 7, 6.5%; p = 0.027) and non-orthopedic surgery (orthopedic 9, 4.0% vs. non-orthopedic 35, 26.9%; p < 0.001). Conclusion: there was a significant discrepancy between the number of requests for blood reservation and its real use and an increased time between reservation requests and their arrival at the TA.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
World Health Organization. WHO Guidelines for Safe Surgery 2009: Safe Surgery Saves Lives. WHO; 2009 [cited 22 Nov 2021]. Available from: https://www.who.int/teams/integrated-health-services/patient-safety/research/safe-surgery
Oliveira EM, Reis IA. What are the perspectives for blood donations and blood component transfusion worldwide? A systematic review of time series studies. Sao Paulo Med J. 2020;138(1):54-9https://doi.org/10.1590/1516-3180.2019.0415.r1.06112019
Alves JL, Neto CLBG, Hékis HR, Contreras RC, Lins HWC, Melo ASP. Proposta de um novo protocolo de reservas de hemocomponentes para cirurgias em um hospital universitário de Recife-Pernambuco. Rev Bras Inov Tecnol Saúde. 2019:30. https://doi.org/10.18816/r-bits.v8i4.15647
Brasil, Ministério da Saúde, Agência Nacional de Vigilância Sanitária. Resolução RDC no 34, de 11 de junho de 2014. Dispõe sobre as Boas Práticas no Ciclo do Sangue [published online 2011; cited 12 Sep 2023]. Availabe from: https://bit.ly/3PX105U
Belayneh T, Messele G, Abdissa Z, Tegene B. Blood Requisition and Utilization Practice in Surgical Patients at University of Gondar Hospital, Northwest Ethiopia. J Blood Transfus. 2013;2013:758910. https://doi.org/10.1155/2013/758910
McClain CM, Hughes J, Andrews JC, Blackburn J, Sephel S, France D, et al. Blood ordering from the operating room: turnaround time as a quality indicator. Transfusion. 2013;53(1):41-8. https://doi.org/10.1111/j.1537-2995.2012.03670.x
Isidoro REC, Silva KFN, Oliveira JF, Barichello E, Pires PS, Barbosa MH. Solicitação de reserva e preditores para hemotransfusão em cirurgias eletivas de fratura de fêmur. Texto Contexto Enferm. 2019;28:e20180129. https://doi.org/10.1590/1980-265x-tce-2018-0129
Zewdie K, Genetu A, Mekonnen Y, Worku T, Sahlu A, Gulilalt D. Efficiency of blood utilization in elective surgical patients. BMC Health Serv Res. 2019;19(1):804. https://doi.org/10.1186/s12913-019-4584-1
Marcondes SS, Carrareto AR, Zago-Gomes MP, Orletti MPSV, Novaes ACZL. Evaluation of the use of blood in surgeries as a tool to change patterns for requesting blood product reserves. Clinics. 2019;74:e652. https://doi.org/10.6061/clinics/2019/e652
Motulsky HJ, Brown RE. Detecting outliers when fitting data with nonlinear regression - a new method based on robust nonlinear regression and the false discovery rate. BMC Bioinformatics. 2006;7(1):123. https://doi.org/10.1186/1471-2105-7-123
Lobo SM, Vieira SR, Knibel MF, et al. Anemia e transfusões de concentrados de hemácias em pacientes graves nas UTI brasileiras (pelo FUNDO-AMIB). Rev Bras Ter Intens. 2006;18(3):234-41. https://doi.org/10.1590/S0103-507X2006000300004
Lima LP de, Menezes KP, Gadelha D de L, et al. Perfil de transfusão sanguínea e hemocomponentes em um hospital de urgência em Rio Branco. South Am J Basic Educ Tech Technolol. 2021;1(8):248-62.
Sekine L, Wirth LF, Faulhaber GAM, Seligman BGS. Análise do perfil de solicitações para transfusão de hemocomponentes no Hospital de Clínicas de Porto Alegre no ano de 2005. Rev Bras Hematol Hemot. 2008;30(3):208-12. https://doi.org/10.1590/S1516-84842008000300009
Neves MSA, Delgado RB. Suporte hemoterápico ao paciente em emergência médica. Rev Med Minas Gerais. 2010;4(20):568-577. Available from: https://bit.ly/45RrnlC
Bastos SL, Martins JCC, Oliveira ML, et al. Uso de hemocomponentes em hospital de médio porte em Belo Horizonte, Minas Gerais. Rev Med Minas Gerais. 2014;Supl 6(24):S54-60. https://doi.org/10.5935/2238-3182.20140086
SG B, Srinivasan K, Ananthakrishnan N, Jayanthi S, Ravishankar M. Blood utilization in elective surgery - Requirements, ordering and transfusion practices. Nat Med J India. 1997;4(10):164-8.
Yazdi AP, Alipour M, Jahanbakhsh SS, Gharavifard M, Taghavi M. A Survey of Blood Request Versus Blood Utilization at a University Hospital in Iran. Arch Bone Jt Surg. 2016;4(1):75-9.
Shrestha AN, Aryal BB, Poudel A, et al. Blood transfusion practices in a tertiary care hospital in Nepal. J Pathology Nepal. 2020;10(2):1728-32. https://doi.org/10.3126/jpn.v10i2.30424
Adegboye MB, Kadir DM. Maximum surgical blood ordering schedule for common orthopedic surgical procedures in a tertiary hospital in North Central Nigeria. J Orthop Trauma Surg Rel Res. 2018;1(13):6-9.
Novis DA, Friedberg RC, Renner SW, Meier FA, Walsh MK. Operating Room Blood Delivery Turnaround Time. Arch Pathol Lab Med. 2002;126(8):909-14. https://doi.org/10.5858/2002-126-0909-ORBDTT
Pati HP, Singh G. Turnaround Time (TAT): Difference in Concept for Laboratory and Clinician. Indian J Hematol Blo. 2014;30(2):81-4. https://doi.org/10.1007/s12288-012-0214-3
Agnihotri N, Agnihotri A. Turnaround Time for Red Blood Cell Transfusion in the Hospitalized Patient: A Single-Center "Blood Ordering, Requisitioning, Blood Bank, Issue (of Blood), and Transfusion Delay" Study. Indian J Crit Care Med. 2018;22(12):825-30. https://doi.org/10.4103/ijccm.IJCCM_403_18
Lee AJ, Kim SG. Analysis of Turnaround Time for Intraoperative Red Blood Cell Issues: A Single-Center Study. Lab Med. 2017;48(3):277-81. https://doi.org/10.1093/labmed/lmx016
Como JJ, Dutton RP, Scalea TM, Edelman BB, Hess JR. Blood transfusion rates in the care of acute trauma. Transfusion. 2004;44(6):809-13. https://doi.org/10.1111/j.1537-2995.2004.03409.x
Silva EM, Vieira CA, Silva FO, Ferreira EV. Desafios da enfermagem diante das reações transfusionais. Rev Enferm UERJ. 2014;25(0):e11552. https://doi.org/10.12957/reuerj.2017.11552
Yazer MH, Deandrade DS, Triulzi DJ, Wisniewski MK, Waters JH. Electronic enhancements to blood ordering reduce component waste. Transfusion. 2016;56(3):564-70. https://doi.org/10.1111/trf.13399
Brener S, Carvalho RVF, Ferreira ÂM, Silva MMF, Valle MCR, Moraes-Souza H. Physical and operational infrastructure of transfusion services of the public blood bank network in the State of Minas Gerais, Brazil, 2007/2008. Rev Bras Hematol Hemoter. 2010;32(6):455-62. https://doi.org/10.1590/S1516-84842010000600009