Effects of the exercise mobile app and distance supervision on the functional performance of the older adults. Protocol of a clinical, randomized, controlled trial.
Conteúdo do artigo principal
Resumo
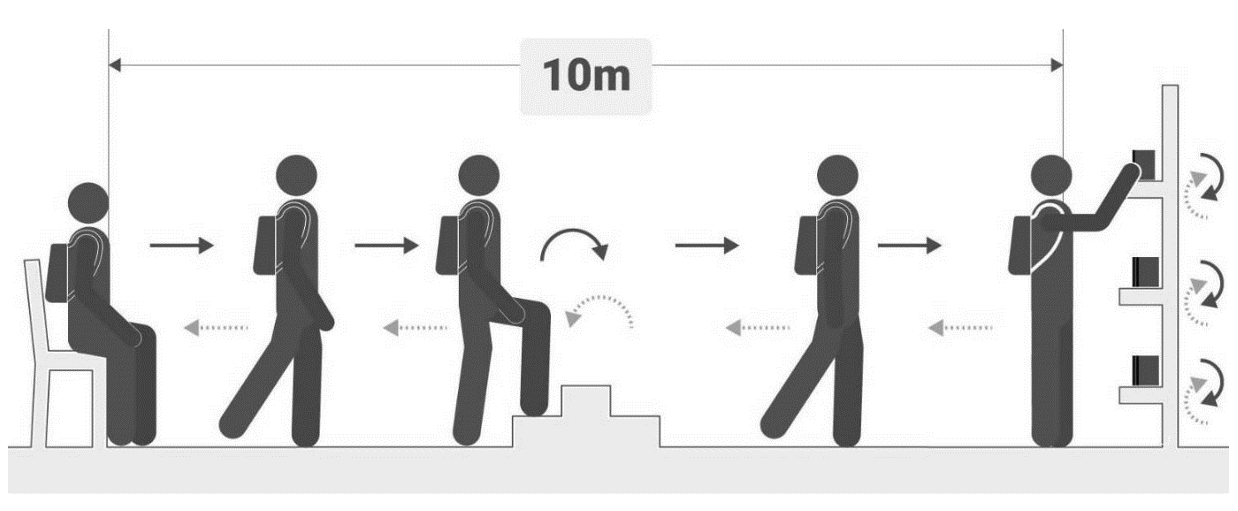
Objective: To check the effects of the exercise mobile app with face-to-face and distance supervision on the functional performance, postural balance, and lower limb strength of older adults. Methods: This is a protocol of a controlled, randomized, and blind clinical trial in which we will recruit older adults of both genders, who will be randomized into two types of training: a control group (exercises using a mobile app with face-to-face monitoring by the therapist) and an experimental group (exercises with a mobile app without face-to-face monitoring by the therapist). The training will be carried out with the free app "Exercício para idosos", which should be installed on the participants' smartphones. The participants should do the proposed exercises three times a week for eight consecutive weeks. The evaluations will be conducted in person pre-training and after the 12th and 24th sessions. Functional performance, postural balance, and lower limb strength will be assessed. The data in each evaluation will be compared as well as the difference between the groups. It is believed that physical exercise apps for older people will benefit both groups by improving functional capacity, postural balance, and lower limbs of older adults.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
Lowry KA, Vallejo AN, Studenski SA. Successful aging as a continuum of functional independence: lessons from physical disability models of aging. Aging Dis. 2012;3(1):5-15. PMID: 22500268 PMCID: PMC3320804
Organização Mundial da Saúde. Relatório Mundial de Envelhecimento e Saúde. Organ Mund Saúde. Geneva: OMS; 2015 [cited 2022 Jun4]. 30 p. Available from: https://bit.ly/3Nm0I7i
Theou O, Stathokostas L, Roland KP, Jakobi JM, Patterson C, Vandervoort AA, et al. The effectiveness of exercise interventions for the management of frailty: A systematic review. J Aging Res .2011;2011:569194. https://doi.org/10.4061/2011/569194
Tarazona-Santabalbina FJ, Gómez-Cabrera MC, Pérez-Ros P, Martínez-Arnau FM, Cabo H, Tsaparas K, et al. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: a randomized clinical trial. J Am Med Dir Assoc. 2016;17(5):426-33. https://doi.org/10.1016/j.jamda.2016.01.019
Jardim NYV, Bento-Torres NVO, Costa VO, Carvalho JPR, Pontes HTS, Tomás AM, et al. Dual-task exercise to improve cognition and functional capacity of healthy older adults. Front Aging Neurosci. 2021;13:589299. https://doi.org/10.3389/fnagi.2021.589299
Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA. 2014;311(23):2387-96. https://doi.org/10.1001/jama.2014.5616
Fleg JL. Aerobic exercise in the elderly: a key to successful aging. Discov Med. 2012 Mar;13(70):223-8. PMID: 22463798
Recio-Rodriguez JI, Agudo-Conde C, Martin-Cantera C, González-Viejo M, Fernandez-Alonso MC, Arietaleanizbeaskoa MS, et al. Short-term effectiveness of a mobile phone app for increasing physical activity and adherence to the mediterranean diet in primary care: A randomized controlled trial (EVIDENT II study). J Med Internet Res. 2016;18(12):e331. https://doi.org/10.2196/jmir.6814
Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, Newell J, et al. Effectiveness of a smartphone application to promote physical activity in primary care: The SMART MOVE randomised controlled trial. Br J Gen Pract. 2014;64(624):e384-91. https://doi.org/10.3399/bjgp14X680461
Nikitina S, Didino D, Baez M, Casati F. Feasibility of virtual tablet-based group exercise among older adults in Siberia: Findings from two pilot trials. JMIR Mhealth Uhealth. 2018;6(2):e40. https://doi.org/10.2196/mhealth.7531
Elavsky S, Knapova L, Klocek A, Smahel D. Mobile health interventions for physical activity, sedentary behavior, and sleep in adults aged 50 years and older: a systematic literature review. J Aging Phys Act. 2019;27(4):565-93. https://doi.org/10.1123/japa.2017-0410
Wang F, Kream RM, Stefano GB. Long-term respiratory and neurological sequelae of COVID-19. Med Sci Monit. 2020;26. https://doi.org/10.12659/MSM.928996
Shelkey M, Wallace M. Katz Index of Independence in Activities of Daily Living. J Gerontol Nurs. 1999;25(3):8-9. https://doi.org/10.3928/0098-9134-19990301-05
Brucki SMDD, Nitrini R, Caramelli P, Bertolucci PHFF, Okamoto IH, Nitrin R, et al. Sugestões para o uso do mini-exame do estado mental no Brasil. Arq Neuropsiquiatr. 2003;61(3B):777-81. https://doi.org/10.1590/S0004-282X2003000500014
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. Inventory for Measuring Depression. Arch Gen Psychiatry. 1961;4:561-71. https://doi.org/10.1001/archpsyc.1961.01710120031004
Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep. 1991;14(4):331-8. PMID: 1947597
Skumlien S, Hagelund T, Bjørtuft Ø, Ryg MS. A field test of functional status as performance of activities of daily living in COPD patients. Respir Med. 2006;100(2):316-23. https://doi.org/10.1016/j.rmed.2005.04.022
Gomes BT. Validação e reprodutibilidade do teste de atividade de vida diária-Glittre para avaliar a capacidade funcional de idosos [Dissertation]. São Paulo, SP: Nove de Julho University; 2018 [cited 2022 Jun 4]. Available from: http://bibliotecatede.uninove.br/handle/tede/2305
Anson E, Thompson E, Ma L, Jeka J. Reliability and fall risk detection for the BESTest and Mini-BESTest in older adults. J Geriatr Phys Ther. 2019;42(2):81-5. https://doi.org/10.1519/jpt.0000000000000123
Bohannon RW, Bubela DJ, Magasi SR, Wang YC, Gershon RC. Sit-to-stand test: Performance and determinants across the age- span. Isokinet Exerc Sci. 2010;18(4):235-40. https://doi.org/10.3233/IES-2010-0389
Botoseneanu A, Ambrosius WT, Beavers DP, De Rekeneire N, Anton S, Church T, et al. Prevalence of metabolic syndrome and its association with physical capacity, disability, and self-rated health in Lifestyle Interventions and Independence for Elders Study participants. J Am Geriatr Soc. 2015;63(2):222-32. https://doi.org/10.1111/jgs.13205
Bray NW, Smart RR, Jakobi JM, Jones GR. Exercise prescription to reverse frailty. Appl Physiol Nutr Metab. 2016;41(10):1112-6. https://doi.org/10.1139/apnm-2016-0226
Paterson DH, Jones GR, Rice CL. Le vieillissement et l'activité physique : données sur lesquelles fonder des recommandations relatives à l'exercice à l'intention des adultes âgés [Aging and physical activity data on which to base recommendations for exercise in older adults]. Appl Physiol Nutr Metab. 2007;32 Suppl 2F:S75-S171. French. https://doi.org/10.1139/h07-165
Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021;55(19):1099-105. https://doi.org/10.1136/bjsports-2021-104080