Antipsychotic-induced movement disorders: integrative review
Main Article Content
Abstract
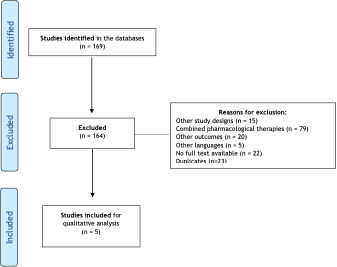
Objective: To identify movement disorders induced by antipsychotics. Methods: We selected clinical trials from MEDLINE and LILACS databases without publication date restriction. Studies of antipsychotics as a pharmacological intervention, compared or not to other interventions were included (combined treatments were not included). The primary outcome was movement disorders. Two independent reviewers analyzed the studies and summarized them in an electronic spreadsheet. We assessed the quality of the selected studies using the PEDro scale. Results: Five studies were included in this review. In these studies, it was possible to identify the main psychiatric symptoms and their severity, as well as dyskinetic movements. When a reduction in dyskinetic movements was observed in treatments with both atypical and typical antipsychotics, there were adverse effects. Those included excessive sedation, loss of body mass, vomiting, and leukocytopenia. Conclusion: This study verified the findings in literature on the effects of antipsychotics, including the type of medication, dosage, and form of administration, as well as instruments used to assess the outcome related to movement disorders. It was not possible to determine the best therapeutic dose for managing the disorders due to the significant distinction in dosages and medications. All five studies had some effect related to the drug use or its withdrawal.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
World Health Organization (WHO). Mental health: strengthening our response [Internet]. Geneva: WHO; 2022 Jun 17 [cited 2022 Aug 05]. Available from: https://bit.ly/3P7bMFg
World Health Organization (WHO). The World Health Report 2001: Mental Health: New Understanding, New Hope [Internet]. Lisboa: WHO; 2001 [cited 2022 Aug 05]. Available from: https://bit.ly/3C1Pn9N
World Health Organization (WHO). Mental health. [Internet]. WHO; 2022 Jul 8 [cited 2022 Aug 5]. Available from: https://bit.ly/3QpKVW0
GBD Compare | Viz Hub [Internet]. Institute for Health Metrics and Evaluation. [cited 2022 Aug 5] Available from: http://vizhub.healthdata.org/gbd-compare
Brasil, Ministério da Saúde, Secretaria de Atenção à Saúde. Saúde mental no SUS: os centros de atenção psicossocial [Internet]. Brasília, DF: Secretaria de Atenção à Saúde; 2004 [cited 2022 Aug 5]. Available from: https://bit.ly/3JOpv33
Ceraso A, Lin JJ, Schneider-Thoma J, Siafis S, Tardy M, Komossa K, et al. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2020;8:CD008016. https://doi.org/10.1002/14651858.CD008016.pub3 DOI: https://doi.org/10.1002/14651858.CD008016.pub3
National Institute of Mental Health. Schizophrenia [Internet]. Bethesda, MD: NIH; [revised 2021; cited 2022 Aug 5]. Available from: https://bit.ly/3A0VedX
Frederico WA, Oga S, Pequeno M, Taniguchi S. Efeitos colaterais extrapiramidais como consequência do tratamento com neurolépticos. Einstein [Internet]. 2008 [cited 2022 Aug 5];6(1):51-5. Available from: https://bit.ly/3JAat0y
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939-51. https://doi.org/10.1016/S0140-6736(19)31135-3 DOI: https://doi.org/10.1016/S0140-6736(19)31135-3
McIntyre RS, Berk M, Brietzke E, Goldstein BI, López-Jaramillo C, Kessing LV, et al. Bipolar disorders. Lancet. 2020;396(10265):1841-56. https://doi.org/10.1016/S0140-6736(20)31544-0 DOI: https://doi.org/10.1016/S0140-6736(20)31544-0
Carbon M, Kane JM, Leucht S, Correll CU. Tardive dyskinesia risk with first- and second-generation antipsychotics in comparative randomized controlled trials: a meta-analysis. World Psychiatry. 2018;17(3):330-40. https://doi.org/10.1002/wps.20579 DOI: https://doi.org/10.1002/wps.20579
Demyttenaere K, Detraux J, Racagni G, Vansteelandt K. Medication-induced akathisia with newly approved antipsychotics in patients with a severe mental illness: a systematic review and meta-analysis. CNS Drugs. 2019;33(6):549-66. https://doi.org/10.1007/s40263-019-00625-3 DOI: https://doi.org/10.1007/s40263-019-00625-3
Mehta SH, Morgan JC, Sethi KD. Drug-induced movement disorders. Neurol Clin. 2015;33(1):153-74. https://doi.org/10.1016/j.ncl.2014.09.011 DOI: https://doi.org/10.1016/j.ncl.2014.09.011
Damásio J, Carvalho S. Doenças do movimento induzidas por fármacos. Acta Med Port [Internet]. 2011 [cited 2022 Aug 5];24:915-22. Available from: https://bit.ly/3bzKny9
Almeida JL, Zuppo IF, Castel S, Reis EA, Oliveira HN, Ruas CM. Health-related quality of life in patients treated with atypical antipsychotics. Braz J Psychiatr. 2020;42(6):599-607. https://doi.org/10.1590/1516-4446-2019-0739 DOI: https://doi.org/10.1590/1516-4446-2019-0739
Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. 2016;30(4):662-9. https://doi.org/10.1111/scs.12327 DOI: https://doi.org/10.1111/scs.12327
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546-53. https://doi.org/10.1111/j.1365-2648.2005.03621.x DOI: https://doi.org/10.1111/j.1365-2648.2005.03621.x
Cashin AG, McAuley JH. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother. 2020;66(1):59. https://doi.org/10.1016/j.jphys.2019.08.005 DOI: https://doi.org/10.1016/j.jphys.2019.08.005
Glazer WM, Hafez H. A comparison of masking effects of haloperidol versus molindone in tardive dyskinesia. Schizophr Res. 1990;3(5-6):315-20. https://doi.org/10.1016/0920-9964(90)90016-Z DOI: https://doi.org/10.1016/0920-9964(90)90016-Z
Hong CJ, Chen JY, Chiu HJ, Sim CB. A double-blind comparative study of clozapine versus chlorpromazine on Chinese patients with treatment-refractory schizophrenia. Int Clin Psychopharmacol. 1997;12(3):123-30. https://doi.org/10.1097/00004850-199705000-00001 DOI: https://doi.org/10.1097/00004850-199705000-00001
Malone RP, Maislin G, Choudhury MS, Gifford C, Delaney MA. Risperidone treatment in children and adolescents with autism: short- and long-term safety and effectiveness. J Am Acad Child Adolesc Psychiatry. 2002;41(2):140-7. https://doi.org/10.1097/00004583-200202000-00007 DOI: https://doi.org/10.1097/00004583-200202000-00007
Paleacu D, Barak Y, Mirecky I, Mazeh D. Quetiapine treatment for behavioural and psychological symptoms of dementia in Alzheimer's disease patients: a 6- week, double-blind, placebo-controlled study. Int J Geriatr Psychiatry. 2008;23(4):393-400. https://doi.org/10.1002/gps.1892 DOI: https://doi.org/10.1002/gps.1892
Curson DA, Barnes TR, Bamber RW, Platt SD, Hirsch SR, Duffy JC. Long-term depot maintenance of chronic schizophrenic out-patients: the seven year follow-up of the Medical Research Council fluphenazine/placebo trial. II. The incidence of compliance problems, side-effects, neurotic symptoms and depression. Br J Psychiatry. 1985;146:469-74. https://doi.org/10.1192/bjp.146.5.469 DOI: https://doi.org/10.1192/bjp.146.5.469
Marazziti D, Baroni S, Picchetti M, Piccinni A, Carlini M, Vatteroni E, et al. Pharmacokinetics and pharmacodynamics of psychotropic drugs: effect of sex. CNS Spectr. 2013;18(3):118-27. https://doi.org/10.1017/S1092852912001010 DOI: https://doi.org/10.1017/S1092852912001010
Moyer AM, Matey ET, Miller VM. Individualized medicine: Sex, hormones, genetics, and adverse drug reactions. Pharmacol Res Perspect. 2019;7(6):e00541. https://doi.org/10.1002/prp2.541 DOI: https://doi.org/10.1002/prp2.541
Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009;48(3):143-57. https://doi.org/10.2165/00003088-200948030-00001 DOI: https://doi.org/10.2165/00003088-200948030-00001
Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37. https://doi.org/10.3389/fnins.2015.00037 DOI: https://doi.org/10.3389/fnins.2015.00037
Cersosimo MG, Benarroch EE. Estrogen actions in the nervous system: Complexity and clinical implications. Neurology. 2015;85(3):263-73. https://doi.org/10.1212/WNL.0000000000001776 DOI: https://doi.org/10.1212/WNL.0000000000001776
González-Rodríguez A, Seeman MV. Pharmacotherapy for schizophrenia in postmenopausal women. Expert Opin Pharmacother. 2018;19(8):809-21. https://doi.org/10.1080/14656566.2018.1465563 DOI: https://doi.org/10.1080/14656566.2018.1465563
Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4(1):8-9. https://doi.org/10.1016/S2215-0366(16)30348-0 DOI: https://doi.org/10.1016/S2215-0366(16)30348-0
Castle DJ. Women and schizophrenia: An epidemiological perspective. In: Castle DJ, McGrath J, Kulkarni J. Women and schizophrenia. American Psychological Association: Cambridge University Press; 2000. pp.19-33.
Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161(8):1324-33. https://doi.org/10.1176/appi.ajp.161.8.1324 DOI: https://doi.org/10.1176/appi.ajp.161.8.1324
Chokhawala K, Stevens L. Antipsychotic Medications. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Brasil, Ministério da Saúde, Departamento de Assistência Farmacêutica e Insumos Estratégicos. Relação nacional de medicamentos essenciais [Internet]. MS; Brasília, DF: 2022 [cited 2022 Aug 5]. Available from: https://bit.ly/3Su1X7c
Maayan N, Quraishi SN, David A, et al. Fluphenazine decanoate (depot) and enanthate for schizophrenia. Cochrane Database Syst Rev. 2015;(2):CD000307. https://doi.org/10.1002/14651858.CD000307.pub2 DOI: https://doi.org/10.1002/14651858.CD000307.pub2
Bagnall A, Fenton M, Kleijnen J, Lewis R. Molindone for schizophrenia and severe mental illness. Cochrane Database Syst Rev. 2007;(1):CD002083. https://doi.org/10.1002/14651858.CD002083.pub2 DOI: https://doi.org/10.1002/14651858.CD002083.pub2
Masuda T, Misawa F, Takase M, Kane JM, Correll CU. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry. 2019;76(10):1052-62. https://doi.org/10.1001/jamapsychiatry.2019.1702 DOI: https://doi.org/10.1001/jamapsychiatry.2019.1702
Jayaram MB, Hosalli P, Stroup S. Risperidone versus olanzapine for schizophrenia. Cochrane Database Syst Rev. 2006;(2):CD005237. https://doi.org/10.1002/14651858.CD005237.pub2 DOI: https://doi.org/10.1002/14651858.CD005237.pub2
Suttajit S, Srisurapanont M, Xia J, Suttajit S, Maneeton B, Maneeton N. Quetiapine versus typical antipsychotic medications for schizophrenia. Cochrane Database Syst Rev. 2013;(5):CD007815. https://doi.org/10.1002/14651858.CD007815.pub2 DOI: https://doi.org/10.1002/14651858.CD007815.pub2
Guy W. ECDEU assessment manual for psychopharmacology [Internet]. Rev. 1976. The Open Library. Rockville, Md: U.S. Dept of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. Available from: https://bit.ly/3P5jwrx
Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11-19. https://doi.org/10.1111/j.1600-0447.1970.tb02066.x DOI: https://doi.org/10.1111/j.1600-0447.1970.tb02066.x
Chouinard P, Ross-Chouinard A, Lawrence A, Barry J. The Extrapyramidal Symptom Rating Scale. Canad J Neurol Sci. 1980 [cied 2022 Aug 5];7(3):233. Available from: https://bit.ly/3JwHRp3
Webster DD. Critical analysis of the disability in Parkinson's disease. Mod Treat. 1968;5(2):257-82. PMId:5655944
Bryan EJ, Purcell MA, Kumar A. Zuclopenthixol dihydrochloride for schizophrenia. Cochrane Database Syst Rev. 2017;11(11):CD005474. https://doi.org/10.1002/14651858.CD005474.pub2 DOI: https://doi.org/10.1002/14651858.CD005474.pub2
BCE Vasconcelos. O cegamento na pesquisa científica. Rev Cir Traumatol Buco-Maxilo-Fac [Internet]. 2016 [cied 2022 Aug 5];16(1):5. Available from: https://bit.ly/3zYcAbl