Distúrbios do movimento induzidos pelo uso de antipsicóticos: revisão integrativa
Conteúdo do artigo principal
Resumo
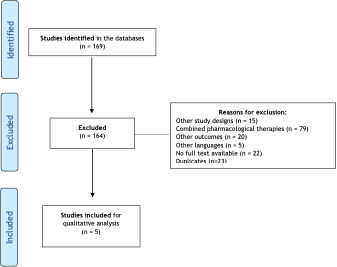
Objetivo: Identificar os distúrbios do movimento induzidos pelo uso de antipsicóticos. Métodos: Foram selecionados ensaios clínicos nas bases de dados MEDLINE e LILACS, sem restrição de data de publicação. Foram incluídos estudos de tratamento com antipsicóticos como intervenção farmacológica comparado ou não a outras intervenções (tratamentos combinados não foram incluídos). O desfecho principal foram os distúrbios do movimento. Os artigos foram analisados por dois revisores independentes e sumarizados em uma planilha eletrônica. A qualidade dos artigos foi avaliada pela escala PEDro. Resultados: Foram incluídos cinco artigos nesta revisão. Nesses estudos foi possível identificar os principais sintomas psiquiátricos e sua severidade, assim como os movimentos discinéticos. Ainda assim, quando apresentaram redução dos movimentos discinéticos tanto nos tratamentos com antipsicóticos atípicos quanto típicos, houve efeitos adversos, como sedação excessiva, perda da massa corporal, vômitos, leucocitopenia de forma isolada. Conclusão: O presente estudo verificou os achados encontrados na literatura sobre os efeitos dos antipsicóticos, incluindo o tipo de medicação, posologia e forma de administração, bem como os instrumentos utilizados para a avaliação do desfecho relacionado aos distúrbios do movimento. Não foi possível verificar a melhor dose terapêutica para o manejo dos distúrbios, devido a grande distinção nas dosagens e medicações. Todos os cinco artigos incluídos apresentaram algum efeito relacionado à medicação utilizada ou à retirada da mesma.
Detalhes do artigo
Os autores mantêm os direitos autorais e concedem ao HSJ o direito de primeira publicação. A partir de 2024, as publicações serão licenciadas sob a Attribution 4.0 International 
 , permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
, permitindo seu compartilhamento, reconhecendo a autoria e publicação inicial nesta revista.
Os autores estão autorizados a assumir contratos adicionais separadamente para distribuição não exclusiva da versão do trabalho publicada nesta revista (por exemplo, publicação em repositório institucional ou como capítulo de livro), com reconhecimento de autoria e publicação inicial nesta revista.
Os autores são incentivados a publicar e distribuir seu trabalho on-line (por exemplo, em repositórios institucionais ou em sua página pessoal) a qualquer momento após o processo editorial.
Além disso, o AUTOR fica informado e consente que o HSJ possa incorporar seu artigo em bases de dados e indexadores científicos existentes ou futuros, nas condições definidas por estes a cada momento, o que envolverá, pelo menos, a possibilidade de que os titulares de esses bancos de dados podem executar as seguintes ações no artigo.
Referências
World Health Organization (WHO). Mental health: strengthening our response [Internet]. Geneva: WHO; 2022 Jun 17 [cited 2022 Aug 05]. Available from: https://bit.ly/3P7bMFg
World Health Organization (WHO). The World Health Report 2001: Mental Health: New Understanding, New Hope [Internet]. Lisboa: WHO; 2001 [cited 2022 Aug 05]. Available from: https://bit.ly/3C1Pn9N
World Health Organization (WHO). Mental health. [Internet]. WHO; 2022 Jul 8 [cited 2022 Aug 5]. Available from: https://bit.ly/3QpKVW0
GBD Compare | Viz Hub [Internet]. Institute for Health Metrics and Evaluation. [cited 2022 Aug 5] Available from: http://vizhub.healthdata.org/gbd-compare
Brasil, Ministério da Saúde, Secretaria de Atenção à Saúde. Saúde mental no SUS: os centros de atenção psicossocial [Internet]. Brasília, DF: Secretaria de Atenção à Saúde; 2004 [cited 2022 Aug 5]. Available from: https://bit.ly/3JOpv33
Ceraso A, Lin JJ, Schneider-Thoma J, Siafis S, Tardy M, Komossa K, et al. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2020;8:CD008016. https://doi.org/10.1002/14651858.CD008016.pub3 DOI: https://doi.org/10.1002/14651858.CD008016.pub3
National Institute of Mental Health. Schizophrenia [Internet]. Bethesda, MD: NIH; [revised 2021; cited 2022 Aug 5]. Available from: https://bit.ly/3A0VedX
Frederico WA, Oga S, Pequeno M, Taniguchi S. Efeitos colaterais extrapiramidais como consequência do tratamento com neurolépticos. Einstein [Internet]. 2008 [cited 2022 Aug 5];6(1):51-5. Available from: https://bit.ly/3JAat0y
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939-51. https://doi.org/10.1016/S0140-6736(19)31135-3 DOI: https://doi.org/10.1016/S0140-6736(19)31135-3
McIntyre RS, Berk M, Brietzke E, Goldstein BI, López-Jaramillo C, Kessing LV, et al. Bipolar disorders. Lancet. 2020;396(10265):1841-56. https://doi.org/10.1016/S0140-6736(20)31544-0 DOI: https://doi.org/10.1016/S0140-6736(20)31544-0
Carbon M, Kane JM, Leucht S, Correll CU. Tardive dyskinesia risk with first- and second-generation antipsychotics in comparative randomized controlled trials: a meta-analysis. World Psychiatry. 2018;17(3):330-40. https://doi.org/10.1002/wps.20579 DOI: https://doi.org/10.1002/wps.20579
Demyttenaere K, Detraux J, Racagni G, Vansteelandt K. Medication-induced akathisia with newly approved antipsychotics in patients with a severe mental illness: a systematic review and meta-analysis. CNS Drugs. 2019;33(6):549-66. https://doi.org/10.1007/s40263-019-00625-3 DOI: https://doi.org/10.1007/s40263-019-00625-3
Mehta SH, Morgan JC, Sethi KD. Drug-induced movement disorders. Neurol Clin. 2015;33(1):153-74. https://doi.org/10.1016/j.ncl.2014.09.011 DOI: https://doi.org/10.1016/j.ncl.2014.09.011
Damásio J, Carvalho S. Doenças do movimento induzidas por fármacos. Acta Med Port [Internet]. 2011 [cited 2022 Aug 5];24:915-22. Available from: https://bit.ly/3bzKny9
Almeida JL, Zuppo IF, Castel S, Reis EA, Oliveira HN, Ruas CM. Health-related quality of life in patients treated with atypical antipsychotics. Braz J Psychiatr. 2020;42(6):599-607. https://doi.org/10.1590/1516-4446-2019-0739 DOI: https://doi.org/10.1590/1516-4446-2019-0739
Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. 2016;30(4):662-9. https://doi.org/10.1111/scs.12327 DOI: https://doi.org/10.1111/scs.12327
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546-53. https://doi.org/10.1111/j.1365-2648.2005.03621.x DOI: https://doi.org/10.1111/j.1365-2648.2005.03621.x
Cashin AG, McAuley JH. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother. 2020;66(1):59. https://doi.org/10.1016/j.jphys.2019.08.005 DOI: https://doi.org/10.1016/j.jphys.2019.08.005
Glazer WM, Hafez H. A comparison of masking effects of haloperidol versus molindone in tardive dyskinesia. Schizophr Res. 1990;3(5-6):315-20. https://doi.org/10.1016/0920-9964(90)90016-Z DOI: https://doi.org/10.1016/0920-9964(90)90016-Z
Hong CJ, Chen JY, Chiu HJ, Sim CB. A double-blind comparative study of clozapine versus chlorpromazine on Chinese patients with treatment-refractory schizophrenia. Int Clin Psychopharmacol. 1997;12(3):123-30. https://doi.org/10.1097/00004850-199705000-00001 DOI: https://doi.org/10.1097/00004850-199705000-00001
Malone RP, Maislin G, Choudhury MS, Gifford C, Delaney MA. Risperidone treatment in children and adolescents with autism: short- and long-term safety and effectiveness. J Am Acad Child Adolesc Psychiatry. 2002;41(2):140-7. https://doi.org/10.1097/00004583-200202000-00007 DOI: https://doi.org/10.1097/00004583-200202000-00007
Paleacu D, Barak Y, Mirecky I, Mazeh D. Quetiapine treatment for behavioural and psychological symptoms of dementia in Alzheimer's disease patients: a 6- week, double-blind, placebo-controlled study. Int J Geriatr Psychiatry. 2008;23(4):393-400. https://doi.org/10.1002/gps.1892 DOI: https://doi.org/10.1002/gps.1892
Curson DA, Barnes TR, Bamber RW, Platt SD, Hirsch SR, Duffy JC. Long-term depot maintenance of chronic schizophrenic out-patients: the seven year follow-up of the Medical Research Council fluphenazine/placebo trial. II. The incidence of compliance problems, side-effects, neurotic symptoms and depression. Br J Psychiatry. 1985;146:469-74. https://doi.org/10.1192/bjp.146.5.469 DOI: https://doi.org/10.1192/bjp.146.5.469
Marazziti D, Baroni S, Picchetti M, Piccinni A, Carlini M, Vatteroni E, et al. Pharmacokinetics and pharmacodynamics of psychotropic drugs: effect of sex. CNS Spectr. 2013;18(3):118-27. https://doi.org/10.1017/S1092852912001010 DOI: https://doi.org/10.1017/S1092852912001010
Moyer AM, Matey ET, Miller VM. Individualized medicine: Sex, hormones, genetics, and adverse drug reactions. Pharmacol Res Perspect. 2019;7(6):e00541. https://doi.org/10.1002/prp2.541 DOI: https://doi.org/10.1002/prp2.541
Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009;48(3):143-57. https://doi.org/10.2165/00003088-200948030-00001 DOI: https://doi.org/10.2165/00003088-200948030-00001
Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37. https://doi.org/10.3389/fnins.2015.00037 DOI: https://doi.org/10.3389/fnins.2015.00037
Cersosimo MG, Benarroch EE. Estrogen actions in the nervous system: Complexity and clinical implications. Neurology. 2015;85(3):263-73. https://doi.org/10.1212/WNL.0000000000001776 DOI: https://doi.org/10.1212/WNL.0000000000001776
González-Rodríguez A, Seeman MV. Pharmacotherapy for schizophrenia in postmenopausal women. Expert Opin Pharmacother. 2018;19(8):809-21. https://doi.org/10.1080/14656566.2018.1465563 DOI: https://doi.org/10.1080/14656566.2018.1465563
Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4(1):8-9. https://doi.org/10.1016/S2215-0366(16)30348-0 DOI: https://doi.org/10.1016/S2215-0366(16)30348-0
Castle DJ. Women and schizophrenia: An epidemiological perspective. In: Castle DJ, McGrath J, Kulkarni J. Women and schizophrenia. American Psychological Association: Cambridge University Press; 2000. pp.19-33.
Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161(8):1324-33. https://doi.org/10.1176/appi.ajp.161.8.1324 DOI: https://doi.org/10.1176/appi.ajp.161.8.1324
Chokhawala K, Stevens L. Antipsychotic Medications. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Brasil, Ministério da Saúde, Departamento de Assistência Farmacêutica e Insumos Estratégicos. Relação nacional de medicamentos essenciais [Internet]. MS; Brasília, DF: 2022 [cited 2022 Aug 5]. Available from: https://bit.ly/3Su1X7c
Maayan N, Quraishi SN, David A, et al. Fluphenazine decanoate (depot) and enanthate for schizophrenia. Cochrane Database Syst Rev. 2015;(2):CD000307. https://doi.org/10.1002/14651858.CD000307.pub2 DOI: https://doi.org/10.1002/14651858.CD000307.pub2
Bagnall A, Fenton M, Kleijnen J, Lewis R. Molindone for schizophrenia and severe mental illness. Cochrane Database Syst Rev. 2007;(1):CD002083. https://doi.org/10.1002/14651858.CD002083.pub2 DOI: https://doi.org/10.1002/14651858.CD002083.pub2
Masuda T, Misawa F, Takase M, Kane JM, Correll CU. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry. 2019;76(10):1052-62. https://doi.org/10.1001/jamapsychiatry.2019.1702 DOI: https://doi.org/10.1001/jamapsychiatry.2019.1702
Jayaram MB, Hosalli P, Stroup S. Risperidone versus olanzapine for schizophrenia. Cochrane Database Syst Rev. 2006;(2):CD005237. https://doi.org/10.1002/14651858.CD005237.pub2 DOI: https://doi.org/10.1002/14651858.CD005237.pub2
Suttajit S, Srisurapanont M, Xia J, Suttajit S, Maneeton B, Maneeton N. Quetiapine versus typical antipsychotic medications for schizophrenia. Cochrane Database Syst Rev. 2013;(5):CD007815. https://doi.org/10.1002/14651858.CD007815.pub2 DOI: https://doi.org/10.1002/14651858.CD007815.pub2
Guy W. ECDEU assessment manual for psychopharmacology [Internet]. Rev. 1976. The Open Library. Rockville, Md: U.S. Dept of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. Available from: https://bit.ly/3P5jwrx
Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11-19. https://doi.org/10.1111/j.1600-0447.1970.tb02066.x DOI: https://doi.org/10.1111/j.1600-0447.1970.tb02066.x
Chouinard P, Ross-Chouinard A, Lawrence A, Barry J. The Extrapyramidal Symptom Rating Scale. Canad J Neurol Sci. 1980 [cied 2022 Aug 5];7(3):233. Available from: https://bit.ly/3JwHRp3
Webster DD. Critical analysis of the disability in Parkinson's disease. Mod Treat. 1968;5(2):257-82. PMId:5655944
Bryan EJ, Purcell MA, Kumar A. Zuclopenthixol dihydrochloride for schizophrenia. Cochrane Database Syst Rev. 2017;11(11):CD005474. https://doi.org/10.1002/14651858.CD005474.pub2 DOI: https://doi.org/10.1002/14651858.CD005474.pub2
BCE Vasconcelos. O cegamento na pesquisa científica. Rev Cir Traumatol Buco-Maxilo-Fac [Internet]. 2016 [cied 2022 Aug 5];16(1):5. Available from: https://bit.ly/3zYcAbl