Bacilloscopy for leprosy in Brazil's public health system between 2013 and 2022
Main Article Content
Abstract
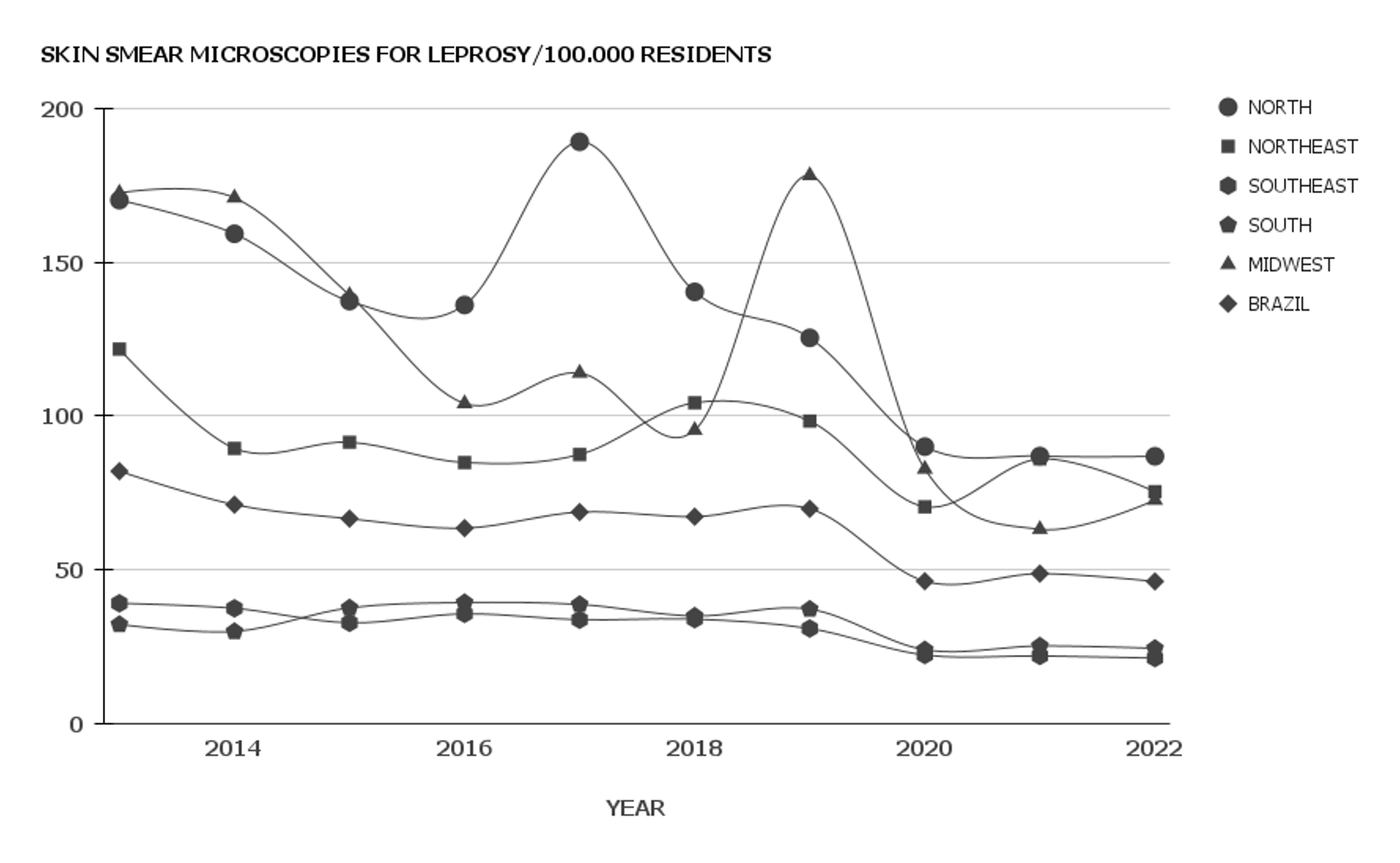
Objective: To evaluate the annual number of skin smear microscopies for leprosy performed in the Unified Health System (SUS) in the last decade. Methods: An ecological, longitudinal, retrospective, and quantitative study was conducted using data from the Ambulatory Information System (SIA/SUS). The number of skin smear microscopies for leprosy per 100,000 residents was estimated for Brazil and its five macroregions, between 2013 and 2022, with a significance level (a) of 5%. Results: More than 1.3 million skin smear microscopies were reported in the last decade in the SUS. The median annual incidence was 67 skin smear microscopies for leprosy per 100,000 residents, with the maximum observed in 2013 (82) and the minimum in 2022 (46). Annual incidences in the North, Central-West, and Northeast macro-regions were significantly higher than the national estimate, whereas in the South and Southeast, they were lower (p <0.05). The temporal trend was considered decreasing for the national estimate (p = 0.002), with an annual percentage variation of -5.6% (95%CI = -3.8%; -8.2%). However, after disregarding the years of the COVID-19 pandemic (2020-2022), the trend became stationary (p = 0.181). Furthermore, the incidence during the pre-pandemic period was significantly higher compared with the third year after the advent of the pandemic in all macro-regions of Brazil (p <0.05). Conclusion: It was possible to conclude that the SUS performed a significant number of skin smear microscopies for leprosy in the last ten years, but there are macro-regional disparities in Brazil and a significant impact of the COVID-19 pandemic.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Chen KH, Lin CY, Su SB, Chen KT. Leprosy: a review of epidemiology, clinical diagnosis, and management. J Trop Med. 2022;2022:8652062. https://doi.org/10.1155/2022/8652062 DOI: https://doi.org/10.1155/2022/8652062
PMid:35832335 PMCid:PMC9273393
Froes-Junior LAR, Sotto MN, Trindade MAB. Leprosy: clinical and immunopathological characteristics. An Bras Dermatol. 2022;97(3):338-47. https://doi.org/10.1016/j.abd.2021.08.006 PMid:35379512 PMCid:PMC9133310 DOI: https://doi.org/10.1016/j.abd.2021.08.006
Gilmore A, Roller J, Dyer JA. Leprosy (Hansen's disease): an update and review. Mo Med. 2023;120(1):39-44. PMid:36860602 PMCid:PMC9970335
Makhakhe L. Leprosy review. S Afr Fam Pract (2004). 2021;63(1):e1-6. https://doi.org/10.4102/safp.v63i1.5311 PMid:34797098 PMCid:PMC8603093 DOI: https://doi.org/10.4102/safp.v63i1.5311
Santos MASD, Mercadante LM, Pegas ES, Kadunc BV. Relationship between bacilloscopy and operational classification of Hansen's disease in patients with reactions. An Bras Dermatol. 2018;93(3):454-6https://doi.org/10.1590/abd1806-4841.20186725 PMid:29924247 PMCid:PMC6001107 DOI: https://doi.org/10.1590/abd1806-4841.20186725
Belotti NCU, Nardi SMT, Paschoal VDA, Montanha JOM, Pedro HSP, Gazetta CE. Laboratory diagnosis of leprosy: two staining methods from bacilloscopy and rapid ml flow test. Int J Mycobacteriol. 2021;10(4):393-7. https://doi.org/10.4103/ijmy.ijmy_206_21 PMid:34916457 DOI: https://doi.org/10.4103/ijmy.ijmy_206_21
Lima LV, Pavinati G, Silva IGP, Moura DRO, Gil NLM, Magnabosco GT. Temporal trend, distribution and spatial autocorrelation of leprosy in Brazil: ecological study, 2011 to 2021. Rev Bras Epidemiol. 2022;25:e220040. https://doi.org/10.1590/1980-549720220040 PMid:36478213
Miguel CB, Mota PB, Afonso BO, Agostinho F, Cazzaniga RA, Abreu MCM, et al. Leprosy morbidity and mortality in Brazil: 2008-2018. Braz J Infect Dis. 2021;25(6):101638. https://doi.org/10.1016/j.bjid.2021.101638 PMid:34756836 PMCid:PMC9392197 DOI: https://doi.org/10.1016/j.bjid.2021.101638
Barbosa-Lima R, Ramos-Silva FF, Santos JCO, Santos DKC, Silva GM, Kameo SY. Leprosy bacilloscopy notifications in the Brazilian Unified Health System and COVID-19 pandemic: an ecological investigation. J Health Biol Sci. 2023 [cited 2023 Dec 14];11(1):1-5. Available from: https://periodicos.unichristus.edu.br/jhbs/article/view/4656 DOI: https://doi.org/10.12662/2317-3076jhbs.v11i1.4656.p1-5.2023
Marques NP, Marques NCT, Cardozo IM, Martelli DRB, Lucena EG, Oliveira EA, et al. Impact of the coronavirus disease 2019 on the diagnoses of Hansen's disease in Brazil. Rev Soc Bras Med Trop. 2021;54:e02512021. https://doi.org/10.1590/0037-8682-0251-2021 PMid:34320132 PMCid:PMC8313100 DOI: https://doi.org/10.1590/0037-8682-0251-2021
Deps P, Collin SM, Andrade VLG. Hansen's disease case detection in Brazil: a backlog of undiagnosed cases due to COVID-19 pandemic. J Eur Acad Dermatol Venereol. 2022;36(10):e754-5. https://doi.org/10.1111/jdv.18307 PMid:35680545 PMCid:PMC9347646 DOI: https://doi.org/10.1111/jdv.18307
Merchán-Hamann E, Tauil PL. Proposal for classifying the different types of descriptive epidemiological studies. Epidemiol Serv Saude. 2021;30(1): e2018126. https://doi.org/10.1590/s1679-49742021000100026 PMid:33950133 DOI: https://doi.org/10.1590/s1679-49742021000100026
Malta M, Cardoso LO, Bastos FI, Magnanini MM, Silva CM. STROBE initiative: guidelines on reporting observational studies. Rev Saude Publica. 2010;44(3):559-65. https://doi.org/10.1590/S0034-89102010000300021 PMid:20549022 DOI: https://doi.org/10.1590/S0034-89102010000300021
Brasil, Ministério da Saúde. Departamento de Informática - Sistema Único de Saúde (DATASUS) [Internet]. Brasília (DF): Ministério da Saúde; 2023 [cited 2023 Jul 6]. Available from: https://datasus.saude.gov.br/
Brasil, Instituto Brasileiro de Geografia e Estatística [Internet]. Brasília (DF): Instituto Brasileiro de Geografia e Estatística; 2023 [cited 2023 Jul 7]. Available from: http://www.ibge.gov.br/
Pagano M, Gauvreau K, Heather M. Principles of bioestatistics. 3a. ed. Boca Raton: CRC Press; 2022. 620p.
Latorre MRDO, Cardoso MRA. Time series analysis in epidemiology: an introduction to methodological aspects. Rev Bras Epidemiol. 2001;4(3):145-52. https://doi.org/10.1590/S1415-790X2001000300002 DOI: https://doi.org/10.1590/S1415-790X2001000300002
Antunes JLF, Cardoso MRA. Using time series analysis in epidemiological studies. Epidemiol Serv Saude. 2015;24(3):565-76. https://doi.org/10.5123/S1679-49742015000300024 DOI: https://doi.org/10.5123/S1679-49742015000300024
Brasil, Ministério da Saúde. Resolução n. 510 de 7 de abril de 2016 [Internet]. Dispõe sobre as normas aplicáveis a pesquisas em ciências humanas e sociais. Diário Oficial da União. 2016 mai. 24; Seção 1. p 44.
Martins-Melo FR, Assunção-Ramos AV, Ramos Júnior AN, Alencar CH, Montenegro Júnior RM, Oliveira MLW, et al. Leprosy-related mortality in Brazil: a neglected condition of a neglected disease. Trans R Soc Trop Med Hyg. 2015;109(10):643-52. https://doi.org/10.1093/trstmh/trv069 PMid:26354792 DOI: https://doi.org/10.1093/trstmh/trv069
Silva CLM, Fonseca SC, Kawa H, Palmer DOQ. Spatial distribution of leprosy in Brazil: a literature review. Rev Soc Bras Med Trop. 2017;50(4):439-49. https://doi.org/10.1590/0037-8682-0170-2016 PMid:28954063 DOI: https://doi.org/10.1590/0037-8682-0170-2016
Pescarini JM, Strina A, Nery JS, Skalinski LM, Andrade KVF, Penna MLF, et al. Socioeconomic risk markers of leprosy in high-burden countries: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(7):e0006622. https://doi.org/10.1371/journal.pntd.0006622 PMid:29985930 PMCid:PMC6053250 DOI: https://doi.org/10.1371/journal.pntd.0006622
Lima LV, Pavinati G, Silva IGP, Moura DRO, Gil NL, Magnabosco GT. Temporal trend, distribution and spatial autocorrelation of leprosy in Brazil: ecological study, 2011 to 2021. Rev Bras Epidemiol. 2022;25:e220040. https://doi.org/10.1590/1980-549720220040.2 DOI: https://doi.org/10.1590/1980-549720220040
Brasil, Ministério da Saúde. Protocolo Clínico e Diretrizes Terapêuticas da Hanseníase [Internet]. Brasília: Secretaria de Vigilância em Saúde, Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis; 2022 [citado 7 jul 2023]. Available from: https://bit.ly/3GIT19k
Diniz SPMC, Pereira DLM, Aquino DMC, Oliveira BLCA, Rabelo PPC, Rolim ILTP. Impacto da COVID-19 na assistência às pessoas acometidas pela hanseníase. Rev Enferm Atual In Derme. 2023;97(2):e023078. https://doi.org/10.31011/reaid-2023-v.97-n.2-art.1627 DOI: https://doi.org/10.31011/reaid-2023-v.97-n.2-art.1627
Lopes JGCBS, Silva IM, Leal MGC, Ribeiro AMS, Leitão JCU, Sousa AFDS, et al. Subdiagnóstico de hanseníase no Brasil durante a pandemia da COVID-19. REAMed. 2022;20:e11172. https://doi.org/10.25248/reamed.e11172.2022 DOI: https://doi.org/10.25248/reamed.e11172.2022
Reis ACNF, Oliveira JPM, Gomes HS, Cavalcante NV. Impact of the COVID-19 pandemic on the continued care of leprosy: an integrative review. RSD. 2022;11(14):e339111436490. https://doi.org/10.33448/rsd-v11i14.36490 DOI: https://doi.org/10.33448/rsd-v11i14.36490
Mendonça IMS, Eleres FB, Silva EMS, Ferreira SMB, Sousa GS. Impact of the COVID-19 pandemic on the care of patients with leprosy: an evaluative study from the perspective of the health professional. RSD. 2022;11(2):e4111225459.