Frequency of chromosomal syndromes in the Brazilian population between 2017 and 2021
Main Article Content
Abstract
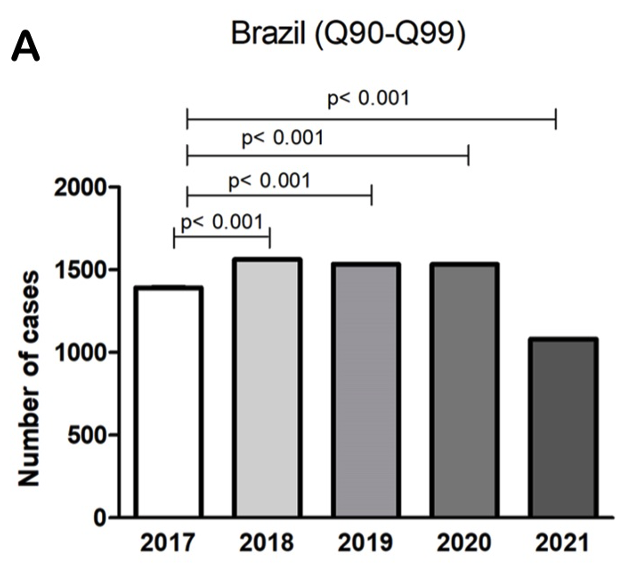
Objective: To evaluate the frequency of chromosomal syndromes in the Brazilian population between 2017 and 2021. Methods: This is an active search of open access databases of the Information System on Live Births (SINASC) from the Brazilian Ministry of Health from 2017 to 2021. For statistical analysis, Analysis of Variance (One-way ANOVA) was followed by the Bonferroni post-test, considering a significant level of p < 0,05. The chi-square test was used for correlation analysis. Results: The underreporting of congenital anomalies in Brazil has decreased over the last few years, showing significant values; however, those numbers varied between regions. The chromosomal syndromes with the highest incidence were Down Syndrome (76.15%), Edwards and Patau Syndromes (14.59%) grouped in the same ICD-10, with the South and Southeast regions, with an average frequency of 0.07%, as the leader in notifications. The maternal variables with a higher incidence of chromosomal syndromes were women over 35 years of age, with 8 to 11 years of schooling, and married. Conclusion: There was a decrease in the value related to underreporting over the years. The data show a disparity in the notification of chromosomal syndromes between regions and outline the maternal profile of a higher incidence of chromosomal syndromes.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Marqui ABT. Chromosomal abnormalities in recurrent miscarriages by conventional karyotyping analysis. Rev Bras Saúde Mater Infant. 2018;18(2):265–76. https://doi.org/10.1590/1806-93042018000200002 DOI: https://doi.org/10.1590/1806-93042018000200002
Moore KL, Persaud TVN. Embriologia Clínica. 11st ed. Rio de Janeiro: Grupo GEN; 2020.
Carvalho AC, Vieira E, Altenhofen TMG, Jung MS. Perfil clínico-epidemiológico dos pacientes atendidos pelo serviço de genética médica do ambulatório materno infantil da universidade do sul de Santa Catarina. Arq Catar Med [Internet]. 2016 [cited 2022 Feb 15];45(2):11–24. Available from: http://acm.org.br/acm/seer/index.php/arquivos/article/view/72
Carmichael SL. Birth defects epidemiology. Eur J Med Gen. 2014 [cited 2022 Jun 17];57(8):355–8. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1769721214000433?via%3Dihub DOI: https://doi.org/10.1016/j.ejmg.2014.03.002
March of Dimes global report on birth defects [Internet]. Marchofdimes.org. 2020 [cited 2022 Jun 17]. Available from: https://www.marchofdimes.org/mission/march-of-dimes-global-report-on-birth-defects.aspx
Bremm JM, Cardoso-dos-Santos AC, Magalhães VS, Medeiros-de-Souza AC, Alves RFS, Araujo VEM, et al. Anomalias congênitas na perspectiva da vigilância em saúde: compilação de uma lista com base na CID-10. Epidemiol Serv Saúde. 2020;29(5):e2020164. https://doi.org/10.1590/S1679-49742020000500015 DOI: https://doi.org/10.1590/s1679-49742020000500015
Vigilância das Anomalias Congênitas [Internet]. Ministério da Saúde. 2022 [cited 2022 Feb 15]. Available from: https://bit.ly/3AWdgxl
Agranonik M, Jung RO. Qualidade dos sistemas de informações sobre nascidos vivos e sobre mortalidade no Rio Grande do Sul, Brasil, 2000 a 2014. Ciênc Saúde Coletiva. 2019;24(5):1945–58. https://doi.org/10.1590/1413-81232018245.19632017 DOI: https://doi.org/10.1590/1413-81232018245.19632017
Brasil. Ministério da Saúde (MS). Portaria n° 199/GM, de 30 de janeiro de 2014. Institui diretrizes para atenção integral às pessoas com doenças raras no Sistema Único de Saúde - SUS. Brasília: Ministério da Saúde; 2014. Available from: https://bit.ly/3QYhbQR
Brasil. Ministério da Saúde (MS). Portaria n° 3.502/GM, de 19 de dezembro de 2017. Institui a Estratégia de fortalecimento das ações de cuidado das crianças suspeitas ou confirmadas para Síndrome Congênita associada à infecção pelo vírus Zika e outras síndromes causadas por sífilis, toxoplasmose, rubéola, citomegalovírus e herpes vírus no Sistema Único de Saúde - SUS. Brasília: Ministério da Saúde; 2017. Available from: https://bit.ly/3wMmKtI
Ministério da Saúde. Painel de Monitoramento de Nascidos Vivos - Natalidade - Painéis de Monitoramento - Centrais de Conteúdos - DASNT - SVS/MS [Internet]. Aids.gov.br. 2018 [cited 2022 Feb 15]. Available from: https://bit.ly/3wKEIg6
World Health Organization. ICD-10 Version:2019 [Internet]. Who.int. 2019 [cited 2022 Mar 25]. Available from: https://icd.who.int/browse10/2019/en
Silva RC, Souza ML, Melo AD. Análise dos Casos Notificados de óbitos fetais por síndromes cromossômicas na região sudeste entre 2000 e 2016: XI Jornada Científica - IFMG Campus Bambuí. 2018 [cited 2022 Feb 15]. Available from: https://bit.ly/3R5HSTM
Cardoso-dos-Santos AC, Medeiros-de-Souza AC, Bremm JM, Alves RFS, Araújo VEM, Leite JCL, et al. Lista de anomalias congênitas prioritárias para vigilância no âmbito do Sistema de Informações sobre Nascidos Vivos do Brasil. Epidemiol Serv Saúde. 2021;30(1):e2020835. https://doi.org/10.1590/S1679-49742021000100030 DOI: https://doi.org/10.1590/s1679-49742021000100030
Meira JGC, Acosta AX. Políticas de saúde pública aplicadas à genética médica no Brasil. Rev Ciênc Méd Biol. 2009;8(2):189. Available from: https://doi.org/10.9771/cmbio.v8i2.4070 DOI: https://doi.org/10.9771/cmbio.v8i2.4070
Oliveira MM, Andrade SSCA, Dimech GS, Oliveira JCG, Malta DC, Rabello Neto DL, et al. Avaliação do Sistema de Informações sobre Nascidos Vivos. Brasil, 2006 a 2010. Epidemiol Serv Saúde. 2015;24(4):629–40. https://doi.org/10.5123/S1679-49742015000400005 DOI: https://doi.org/10.5123/S1679-49742015000400005
Fantin C, Santos ML, Carvalho LB, Gomes NM, Souza LN, Sousa GB. Estudo das anomalias cromossômicas ocorridas em uma maternidade nos anos de 2010 a 2014. Cogitare Enferm. 2017;22(1):e48599. http://doi.org/10.5380/ce.v22i1.48599 DOI: https://doi.org/10.5380/ce.v22i1.48599
Toufaily MH, Westgate M-N, Lin AE, Holmes LB. Causes of Congenital Malformations. Birth Def Res. 2018;110(2):87–91. Available from: https://doi.org/10.1002/bdr2.1105 DOI: https://doi.org/10.1002/bdr2.1105
Anderka M, Mai CT, Romitti PA, Copeland G, Isenburg J, Feldkamp ML, et al. Development and implementation of the first national data quality standards for population-based birth defects surveillance programs in the United States. BMC Public Health. 2015;15(1):925. https://doi.org/10.1186/s12889-015-2223-2 DOI: https://doi.org/10.1186/s12889-015-2223-2
World Health Organization. Congenital anomalies [Internet]. Who.int. World Health Organization: WHO; 2020 [cited 2022 Feb 15]. Available from: https://bit.ly/3KxWs3X
Guimarães ALS, Barbosa CC, Oliveira CM, Maia LTS, Bonfim CV. Relationship of databases of live births and infant deaths for analysis of congenital malformations. Rev Bras Saude Mater Infant. 2019;19(4):917–24. https://doi.org/10.1590/1806-93042019000400010 DOI: https://doi.org/10.1590/1806-93042019000400010
Brasil, Conselho Nacional de Secretários de Saúde. Nota técnica 05/2007. Política nacional de atenção integral em genética clínica. Available from: www.conass.org.br/admin/arquivos/NT05-07.pdf
Rankin J. Prevalence of congenital anomalies in five British regions, 1991-99. Arch Dis Child Fetal Neonatal Ed [Internet]. 2005 [cited 2022 Jun 14];90(5):F374–9. Available from: https://fn.bmj.com/content/90/5/F374.short DOI: https://doi.org/10.1136/adc.2003.047902
Novoa MC, Burnham TF. Desafios para a universalização da genética clínica: o caso brasileiro. Rev Panam Salud Pública [Internet]. 2011 Jan [cited 2022 Mar 19];29(1):61–8. Available from: https://www.scielosp.org/pdf/rpsp/2011.v29n1/61-68/pt DOI: https://doi.org/10.1590/S1020-49892011000100010
Venâncio AC, Costa RD, Zanenga R, Zanenga D, Pinho GHCO, Galera MF. Anomalias cromossômicas: análise da demanda de 28 anos de um laboratório de citogenética do MT. Rev Amrigs [Internet]. 2020 [cited 2022 Feb 15];64(2):179-185. Available from: https://bit.ly/3TIp5zN
Nielsen J, Wohlert M. Chromosome abnormalities found among 34910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Hum Genet. 1991;87:81–3. https://doi.org/10.1007/BF01213097 DOI: https://doi.org/10.1007/BF01213097
Balkan M, Akbas H, Isi H, Oral D, Turkyılmaz A, Kalkanli S, et al. Cytogenetic analysis of 4216 patients referred for suspected chromosomal abnormalities in Southeast Turkey. Genet Mol Res [Internet]. 2010 [cited 2022 Feb 15]; 9(2):1094-1103. Available from: https://bit.ly/3TvvWMJ DOI: https://doi.org/10.4238/vol9-2gmr827
Miziara RC, Marques SBS, Marques JHS, Rezende C, Aquino R, Cury Rodrigues V, et al. The cytogenetic examination as a tool for the diagnosis of chromosomal disorders. Int J Morphol [Internet]. 2011 [cited 2022 Feb 15]; 29(1):57-64. Available from: https://bit.ly/3R4uGP1 DOI: https://doi.org/10.4067/S0717-95022011000100009
Gomes JCO, Dominguetti CP. Fatores de risco da gravidez tardia. Brazilian Journal of Health and Pharmacy [Internet]. 2021 [cited 2022 Feb 15];3(4):1–9. Available from: https://bit.ly/3wJxvwT DOI: https://doi.org/10.29327/226760.3.4-1
Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: A systematic review and meta-analysis. PLOS ONE. 2017;12(10):e0186287. https://doi.org/10.1371/journal.pone.0186287 DOI: https://doi.org/10.1371/journal.pone.0186287
Frederiksen LE, Ernst A, Brix N, Braskhøj Lauridsen LL, Roos L, Ramlau-Hansen CH, et al. Risk of adverse pregnancy outcomes at advanced maternal age. Obst Gynecol. 2018;131(3):457–63. https://doi.org/10.1097/aog.0000000000002504 DOI: https://doi.org/10.1097/AOG.0000000000002504
Cimadomo D, Fabozzi G, Vaiarelli A, Ubaldi N, Ubaldi FM, Rienzi L. Impact of maternal age on oocyte and embryo competence. Front Endocrinol (Lausanne). 2018;9:327. doi: https://doi.org/10.3389/fendo.2018.00327 DOI: https://doi.org/10.3389/fendo.2018.00327
Fritz R, Klugman S, Lieman H, Schulkin J, Taouk L, Castleberry N, et al. Counseling patients on reproductive aging and elective fertility preservation—a survey of obstetricians and gynecologists’ experience, approach, and knowledge. J Assist Reprod Genet. 2018;35(9):1613–21. https://doi.org/10.1007/s10815-018-1273-7 DOI: https://doi.org/10.1007/s10815-018-1273-7
Iriart JAB, Nucci MF, Muniz TP, Viana GB, Aureliano WA, Gibbon S. Da busca pelo diagnóstico às incertezas do tratamento: desafios do cuidado para as doenças genéticas raras no Brasil. Ciênc Saúde Coletiva. 2019;24(10):3637–50. https://doi.org/10.1590/1413-812320182410.01612019 DOI: https://doi.org/10.1590/1413-812320182410.01612019