Evaluation of the social communication of children up to 12 years old with Autism Spectrum Disorder in a Psychosocial Care Center
Main Article Content
Abstract
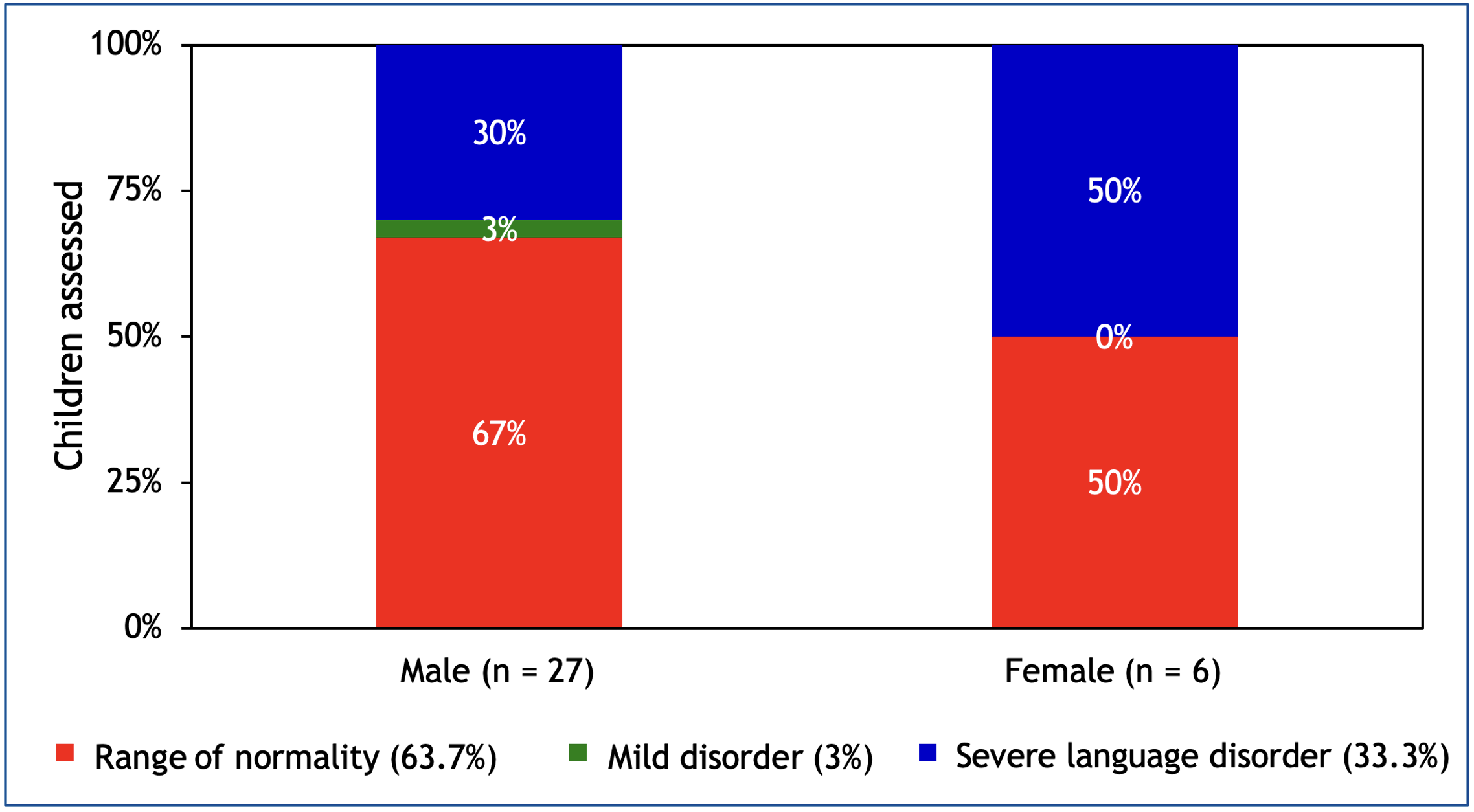
Objective: To characterize social communication in children up to 12 years old diagnosed with Autistic Spectrum Disorder (ASD) treated at the Child Psychosocial Care Center (CAPSi) in Mossoró/RN. Methods: Exploratory, descriptive, quantitative, cross-sectional study conducted at CAPSi in Mossoró/RN. The data collection was based on the application of questionnaires to parents/guardians to characterize their socioeconomic conditions and their perception of their children. The Language Development Assessment (LDA) instrument for children was used, developed to assess the acquisition and development of language content (semantics) and structure (morphology and syntax). The questionnaires were coded, and the data were tabulated for further statistical analysis. Results: 33 children and 73 parents/guardians were studied. Most parents/guardians were female (95.9%), aged 30-39 years (mean age 37.6 years predominantly), with a partner (60%), with high school education (45%), and monthly income around one minimum wage (76.7%), having positive attitudes toward their children and noticing difficulties in their communication. In applying the questionnaire to the children, 63.7% presented results within the normal range, while 3% presented mild and 33.3% severe language alterations. Conclusion: Children with ASD attending CAPSi have language disorders in the pragmatic sublevel, and more than half of the participants did not have morphosyntactic and semantic changes.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
2. Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217-50. Disponível em: http://mail.neurodiversity.com/library_kanner_1943.pdf.
3. Schwartzman JS. Autismo infantil. São Paulo: Memnon; 2003.
4. Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet. 2014;383(9920):896-910. doi: 10.1016/S0140-6736(13)61539-1.
5. Teixeira G. Manual do Autismo. 2a ed. Rio de Janeiro: Best Seller; 2016.
6. Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. MMWR Surveill Summ. 2021;70(SS-11). doi: 10.15585/mmwr.ss7011a1.
7. Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S et al. Global prevalence of autism: A systematic review update. Autism Res. 2022;15(5):778-90. doi: 10.1002/aur.2696.
8. Vorstman JAS, Parr JR, Moreno-De-Luca D, Anney RJL, Nurnberger Jr. JI, Hallmayer JF. Autism genetics: opportunities and challenges for clinical translation. Nat Rev Genet. 2017;18(6):362-76. doi:10.1038/nrg.2017.4.
9. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children: confirmation of high prevalence. Am J Psychiatry. 2005;162(6):1133-41. doi: 10.1176/appi.ajp.162.6.1133.
10. Muhle R, Trentacoste SV, Rapin I. The genetics of autism. Pediatrics. 2004;113:e472-86. doi: 10.1542/peds.113.5.e472.
11. Deng W, Zou X, Deng H, Li J, Tang C, Wang X et al. The Relationship Among Genetic Heritability, Environmental Effects, and Autism Spectrum Disorders: 37 Pairs of Ascertained Twin Study. J Child Neurol. 2015;30(13):1794-99. doi: 10.1177/0883073815580645.
12. Islam MS, Kanak F, Iqbal MA, Islam KF, Al-Mamun A, Uddin MS. Analyzing the Status of the Autism Spectrum Disorder Amid Children with Intellectual Disabilities in Bangladesh. Biomed Pharmacol J. 2018;11(2). doi: 10.13005/bpj/1422.
13. Ruzzo EK, Perez-Cano L, Jung JY, Wang LK, Kashef-Haghighi D, Hartl C et al. Inherited and De Novo Genetic Risk for Autism Impacts Shared Networks. Cell. 2019;178(4):850-866.e26. doi: 10.1016/j.cell.2019.07.015.
14. Whitman TL. O desenvolvimento do autismo: social, cognitivo, linguístico, sensório-motor e perspectivas biológicas. São Paulo: Editora M. Books; 2015.
15. Tager-Flusberg H, Joseph R, Folstein S. Current directions in research on autism. Ment Retard Dev Disabil Res Rev. 2001;7(1):21-9. doi: 10.1002/1098-2779(200102)7:1<21::AID-MRDD1004>3.0.CO;2-3.
16. Reis HIS, Pereira APS, Almeida LS. Características e Especificidades da Comunicação Social na Perturbação do Espectro do Autismo. Rev Bras Educ Espec. 2016;22(3):325-36. doi: 10.1590/S1413-65382216000300002.
17. Ramos AP, Bortagarai FM. A comunicação não-verbal na área da saúde. Rev CEFAC. 2011;14(1):S95-S103. doi: 10.1590/S1516-18462011005000067.
18. Balestro JI, Fernandes FDM. Questionário sobre dificuldades comunicativas percebidas por pais de crianças do espectro do autismo. Rev Soc Bras Fonoaudiol. 2012;17(3):279-86. doi: 10.1590/S1516-80342012000300008.
19. Menezes MLN. ADL: avaliação do desenvolvimento da linguagem. São Paulo: Pró-Fono; 2004.
20. Faé IG, Azevedo PG, Sales ALBC, Ribeiro PC, Mares YS, Melo FM et al. Diagnóstico diferencial entre transtornos de espectro autista e transtorno específico de linguagem receptivo e expressivo: uma revisão integrativa. Rev Med Minas Gerais. 2018;28(Supl.6):e-S280609. doi: 0.5935/2238-3182.20180101.
21. McAuliffe T, Thomas Y, Vaz S, Falkmer T, Cordier R. The experiences of mothers of children with autism spectrum disorder: Managing family routines and mothers’ health and wellbeing. Aust Occup Ther J. 2019;66(1):68-76. doi: 10.1111/1440-1630.12524.
22. Hladik L, Ausderau K, St John B. Experience and perceptions of mothers participating in an in-home, parent-mediated feeding intervention for their child with autism. Am J Occup Ther. 2022;76(Suppl_1):7610510212p1. doi: 10.5014/ajot.2022.76S1-PO212.
23. Cabral CS, Falcke D, Marin AH. Relação Família-Escola-Criança com Transtorno do Espectro Autista: Percepção de Pais e Professoras. Rev Bras Educ Espec. 2021;27(e0156):493-508. doi: 10.1590/1980-54702021v27e0156.
24. Pinto RNM, Torquato IMB, Collet N, Reichert APS, Souza Neto VL, Saraiva AM. Autismo infantil: impacto do diagnóstico e repercussões nas relações familiares. Ver Gaúcha Enferm. 2016;37(3):e61572. doi: 10.1590/1983-1447.2016.03.61572.
25. Passos BC, Kishimoto MSC. O impacto do diagnóstico de Transtorno do Espectro Autista na família e relações familiares. Braz J Develop. 2022;8(1):5827-32. doi: 10.34117/bjdv8n1-394.
26. Silva EF. O impacto financeiro nas famílias que tem diagnóstico de TEA (transtorno do espectro autista) e suas consequências financeiras e econômicas para a sociedade. In: Soares AM, editor. Tópicos Especiais em Ciências da Saúde: teoria, métodos e práticas 4. AyaEditora; 2022. p. 190-201. doi: 10.47573/aya.5379.2.67.16.
27. Costa EF, Cavalcante LIC, Dell’Aglio DD. Language development profile of children in Belem, according to Denver Developmental Screening Test. Rev CEFAC. 2015;17(4):1090-102. doi: 10.1590/1982-0216201517418514.
28. Alencar CN, Costa EF, Cavalcante LIC. Associação entre a Pobreza Familiar e o Desenvolvimento Neuropsicomotor de Crianças na Educação Infantil. Rev Psicol IMED. 2018;10(2):89-102. doi: 10.18256/2175-5027.2018.v10i2.2741.
29. Barbosa PME, Melo JL, Queiroz MAS, Porto ACL, Oliveira LC, Andrade, ISN. Perfil Sociolinguístico e Alimentar de Crianças Assistidas em Creches Públicas e Privadas. Rev Cienc Gerenc. 2019;23(3):244-50. doi: 10.17921/1415-6938.2019v23n3p244-250.
30. Famitafreshi H, Karimian K. Overview of the Recent Advances in Pathophysiology and Treatment for Autism. CNS Neurol Disord Drug Targets. 2018;17(8):590-94. doi: 10.2174/1871527317666180706141654.
31. Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392:508-20. doi: 10.1016/S0140-6736(18)31129-2.
32. Hodges H, Fealko C, Soares N. Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Transl Pediatr. 2020;9(Suppl 1):S55-S65. doi: 10.21037/tp.2019.09.09.
33. Jacquemont S, Coe BP, Hersch M, Duyzend MH, Krumm N, Bergmann S et al. A higher mutational burden in females supports a "female protective model" in neurodevelopmental disorders. Am J Hum Genet. 2014;94(3):415-25. doi: 10.1016/j.ajhg.2014.02.001.
34. Botura C, Machado DO, Marinho ACO, Almeida AN, Ribas LP. Alterações na pragmática de crianças falantes de português brasileiro com diagnóstico de transtorno do espectro autista: uma revisão sistemática. Distúrb Comun. 2021;33(4):627-38. doi: 10.23925/2176-2724.2021v33i4p627-638.
35. Kurita H. Disorders of the autism spectrum. Lancet. 2006;368(9531):179-81. doi: 10.1016/s0140-6736(06)69015-6.
36. Volkmar FR, Chawarska K. Autism in infants: an update. World Psychiatry. 2008;7(1):19-21. doi: 10.1002/j.2051-5545.2008.tb00141.x.