Epidemiological characterization of stroke cases under rehabilitation on the Brazilian Unified Health System in Mossoró, Rio Grande do Norte
Main Article Content
Abstract
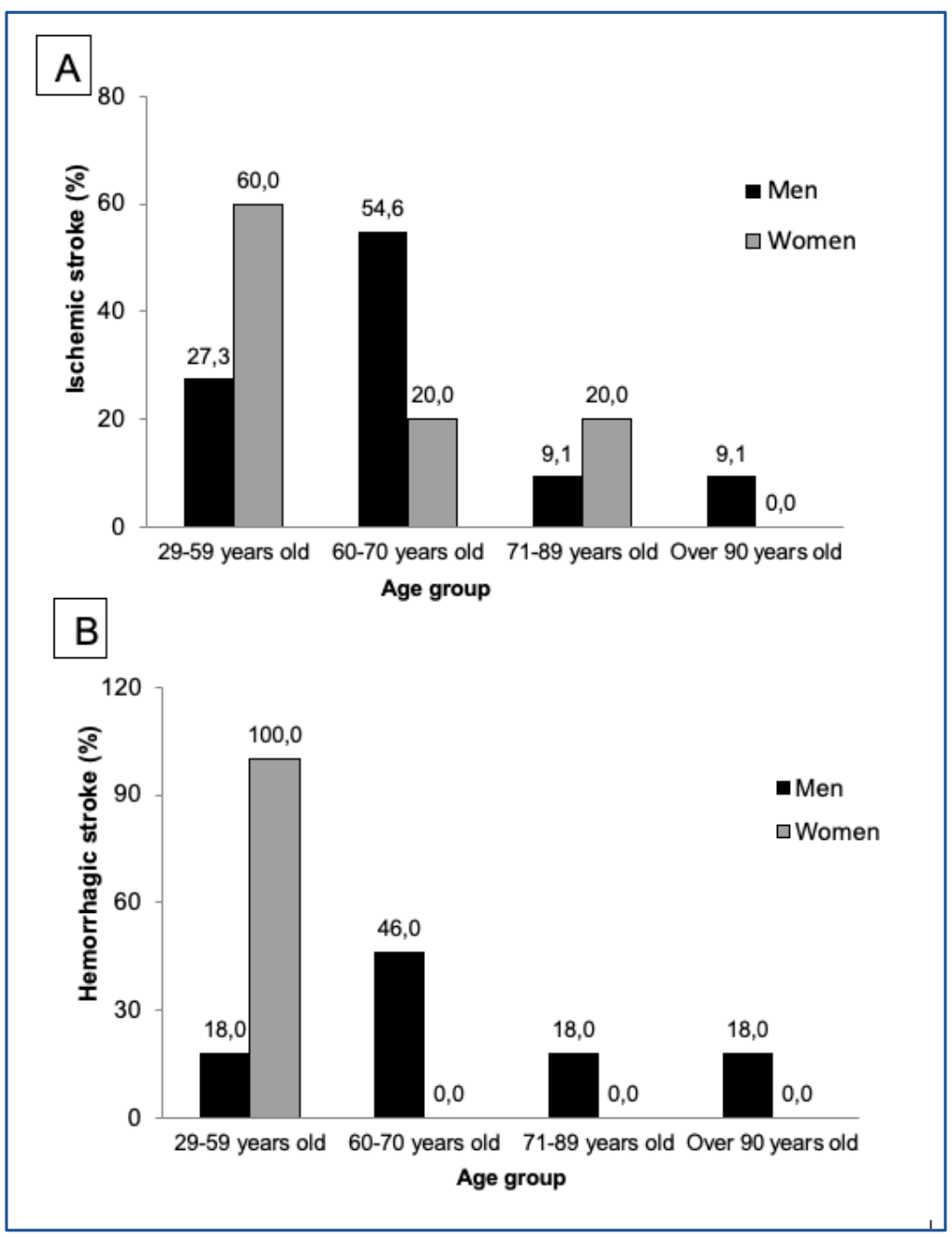
Objectives: To identify the clinical and epidemiological characteristics of patients undergoing treatment for a stroke at the only public rehabilitation clinic in Mossoró/RN (Doctor Ozias Alves de Souza Rehabilitation Center). Methods: Quantitative, prospective, descriptive, cross-sectional, exploratory study, structured from responses to a clinical-epidemiological and sociodemographic questionnaire with 39 items, to assess aspects concerning the profile of patients affected by stroke and undergoing rehabilitation treatment. Results: Twenty-eight individuals with stroke sequelae undergoing treatment at the rehabilitation center were identified, whose clinical-epidemiological characteristics revealed equivalence concerning gender (50% male:female), the predominance of white and brown color/race (46.4% each), and overweight (35.7%). Most of the patients lived in a family environment with a spouse (64.3%), were retired (71.4%), with monthly income between one and two minimum wages (64.3%), with hemiplegic sequelae resulting from the stroke (85.7%) and difficulties in adapting to the current way of life (75%). Conclusion: The present study allows an initial scrutiny of stroke cases in Mossoró/RN and their rehabilitation process. Such data may contribute to a better understanding of issues concerning stroke by government sectors, aiming to improve care and multidisciplinary interventions to provide patients with reinsertion in both work practice and in everyday social relationships.
Article Details
Authors maintain copyright and grant the HSJ the right to first publication. From 2024, the publications wiil be licensed under Attribution 4.0 International 
 , allowing their sharing, recognizing the authorship and initial publication in this journal.
, allowing their sharing, recognizing the authorship and initial publication in this journal.
Authors are authorized to assume additional contracts separately for the non-exclusive distribution of the version of the work published in this journal (e.g., publishing in an institutional repository or as a book chapter), with acknowledgment of authorship and initial publication in this journal.
Authors are encouraged to publish and distribute their work online (e.g., in institutional repositories or on their personal page) at any point after the editorial process.
Also, the AUTHOR is informed and consents that the HSJ can incorporate his article into existing or future scientific databases and indexers, under the conditions defined by the latter at all times, which will involve, at least, the possibility that the holders of these databases can perform the following actions on the article.
References
Brasil, Ministério da Saúde, Secretaria de Atenção à Saúde. Diretrizes de atenção à reabilitação da pessoa com traumatismo cranioencefálico. Brasília, DF: Ministério da Saúde; 2015 [cited 2021 Nov 17]. 130 p. Avaiable from: https://bit.ly/3Cwc6XL
WHO. World Health Statistics 2017: monitoring health for the SDGs, Sustainable Development Goals [Internet]. Geneva: World Health Organization; 2017 [cited 2021 Nov 17]. Vol 3. Available from: https://bit.ly/32ca3ff
Katan M, Luft A. Global Burden of Stroke. Semin Neurol. 2018;38(2):208-11. https://doi.org/10.1055/s-0038-1649503 PMid:29791947
Feigin VL, Mensah GA, Norrving B, Murray CJL, Roth GA, GBD 2013 Stroke Panel Experts Group. Atlas of the Global Burden of Stroke (1990-2013): The GBD Study. Neuroepidemiology 2015;45(3):230-6. https://doi.org/10.1159/000441106 PMid:26505985 PMCid:PMC4630023
Straka M, Trapezanlidis M. Periodontitis and stroke. Neuro Endocrinol Lett. 2013;34(3):200-6. Available from: https://bit.ly/3FqaZe7
Fagundes NCF, Couto RSD, Brandão APT, Lima LAO, Bittencourt LO, Souza-Rodrigues RD et al. Association between tooth loss and stroke: A systematic review. J Stroke Cerebrovasc Dis. 2020;29(8):104873. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104873 PMid:32689647
Hughes AD, Falaschetti E, Witt N, Wijetunge S, McG Thom SA, Tillin T, et al. Association of retinopathy and retinal microvascular abnormalities with stroke and cerebrovascular disease. Stroke. 2016;47(11):2862-4. https://doi.org/10.1161/STROKEAHA.116.014998 PMid:27729577 PMCid:PMC5082730
GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;48:439-58. https://doi.org/10.1016/S1474-4422(19)30034-1
IHME. Instituto de Métrica e Avaliação em Saúde. Estudo de Carga de Doença Global: gerando evidências, informando políticas de saúde. Seattle, Universidade de Washington WA - EUA, 2013 [cited 2021 Nov 17]. Avaiable from: https://bit.ly/3FrONk0
World Health Organization. Health statistics and information systems - Projections of mortality and causes of death, 2015 and 2030. Geneva: WHO;2013
Guzik A, Bushnell C. Stroke epidemiology and risk factor management. Continuum. 2017;23(1):15-39. https://doi.org/10.1212/CON.0000000000000416 PMid:28157742
Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980;58(1):113-30. PMCid:PMC2395894
Instituto Brasileiro de Geografia e Estatística. Indicadores Sociodemográficos e de Saúde no Brasil. Número 25. Rio de Janeiro: IBGE; 2009 [cited 2021 Nov 17]. Avaiable from: https://bit.ly/3DrZySB
Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929-38. https://doi.org/10.1016/S0140-6736(07)61696-1
Lopes JM, Medeiros AJL, Oliveira KBA, Dantas FG. Acidente vascular cerebral isquêmico no Nordeste brasileiro: uma análise temporal de 13 anos de casos de hospitalização. ConScientiae Saúde. 2013;12 (2):321-8. https://doi.org/10.5585/conssaude.v12n2.4100
Instituto Brasileiro de Geografia e Estatística. Censo Demográfico 2010. Questionário Básico CD2010. Avaiable from: https://bit.ly/3qI6VC2
Riberto M, Miyazaki MH, Jucá SSH, Sakamoto H, Pinto PPN, Battistella LR. Validação da versão brasileira da Medida de Independência Funcional. Acta Fisiatr. 2004;11(2):72-6. https://doi.org/10.5935/0104-7795.20040003
Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D'Agostino RB, Wolf PA. The Influence of gender and age on disability following ischemic stroke: the framingham study. J Stroke Cerebrovasc Dis. 2003;12:119-26. https://doi.org/10.1016/S1052-3057(03)00042-9
Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915-26. https://doi.org/10.1016/S1474-4422(08)70193-5
Hiraga A. Gender differences and stroke outcomes. Neuroepidemiology. 2017;48(1-2):61-62. https://doi.org/10.1159/000475451 PMid:28419999
Dupre ME, Lopes RD. Marital history and survival after stroke. J Am Heart Assoc. 2016;5(12):e004647. https://doi.org/10.1161/JAHA.116.004647 PMid:27974292 PMCid:PMC5210404
Engström G, Khan FA, Zia E, Jerntorp I, Pessah-Rasmussen H, Norrving B, et al. Marital dissolution is followed by an increased incidence of stroke. Cerebrovasc Dis. 2004;18(4):318-24. https://doi.org/10.1159/000080770 PMid:15359099
Dupre ME. Race, marital history, and risks for stroke in US older adults. Soc Forces 2016;95(1):439-68. https://doi.org/10.1093/sf/sow040 PMid:29187763 PMCid:PMC5703199
Oliveira GMM, Klein CH, Silva NAS. Mortalidade por doenças cardiovasculares em três estados do Brasil de 1980 a 2006. Rev Panam Salud Publica 2010;19(2):85-93. https://doi.org/10.1590/S1020-49892006000200003 PMid:16551382
Dias KS. Perfil dos indivíduos portadores de acidente vascular cerebral vinculados ao programa de saúde da família no município de Divinópolis-MG: A demanda por cuidados fisioterapêuticos [Dissertação em Promoção de Saúde]. Universidade de Franca; 2006.
Droste DW, Ritter MA, Dittrich R, Heidenreich S, Wichter T, Freund M, et al. Arterial hypertension and ischaemic stroke. Acta Neurol Scand. 2003;107(4):241-51. https://doi.org/10.1034/j.1600-0404.2003.00098.x PMid:12675696
Feigin VL, Norrving B, Mensah GA. Global Burden of Stroke. Circ Res. 2017;120(3):439-48. https://doi.org/10.1161/CIRCRESAHA.116.308413 PMid:28154096
Marianelli M, Marianelli C, Neto TPL. Principais fatores de risco para o AVC isquêmico: uma abordagem descritiva. Braz J Hea Rev. 2020;3:19679-190. https://doi.org/10.34119/bjhrv3n6-344
Gallacher KI, Jani BD, Hanlon P, Nicholl BI, Mair FS. Multimorbidity in stroke. Stroke 2019;50(7):1919-26. https://doi.org/10.1161/STROKEAHA.118.020376 PMid:31233391
Karatepe AG, Guaydin R, Kaya T, Turkmen G. Comorbidity in patients after stroke: Impact on functional outcome. J Rehabil Med. 2008;40(10):831-5. https://doi.org/10.2340/16501977-0269 PMid:19242620
Elkind MS. Stroke in the elderly. Mt Sinai J Med. 2003;70(1):27-37. PMid:12516007
Yousufuddin M, Young N. Aging and ischemic stroke. Aging (Albany NY). 2019;11(9):2542-4. https://doi.org/10.18632/aging.101931 PMid:31043575 PMCid:PMC6535078
Malta DC, Stopa SR, Szwarcwald CL, Gomes NL, Junior JBS, Reis AAC. A vigilância e o monitoramento das principais doenças crônicas não transmissíveis no Brasil - Pesquisa Nacional de Saúde, 2013. Rev Bras Epidemiol. 2015;18(Suppl 2):3-16. https://doi.org/10.1590/1980-5497201500060002 PMid:27008599
Duncan BB, Chor D, Aquino EML, Bensenor IM, Mill JG, Schmidt MI, et al. Doenças Crônicas Não Transmissíveis no Brasil: prioridade para enfrentamento e investigação. Rev Saúde Pública. 2012;46 (Suppl 1):126-34. https://doi.org/10.1590/S0034-89102012000700017 PMid:23532314
Rangel ESS, Belasco AGS, Diccini S. Qualidade de vida de pacientes com acidente vascular cerebral em reabilitação. Acta Paul Enf. 2013;26:205-12. https://doi.org/10.1590/S0103-21002013000200016
Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, et al. Management of adult stroke rehabilitation care: A clinical practice guideline. Stroke. 2005;36(9):e100-43. https://doi.org/10.1161/01.STR.0000180861.54180.FF
Li Y, Wang D, Zhang H, Wang Y, Wu P, Zhang H, et al. Changes of brain connectivity in the Primary Motor Cortex after subcortical stroke. Medicine (Baltimore). 2016;95(6):e2579. https://doi.org/10.1097/MD.0000000000002579 PMid:26871777 PMCid:PMC4753872
Van Kuijk AA, Van der Linde H, Van Limbeek J. Urinary incontinence in stroke patients after admission to a post-acute inpatient rehabilitation program. Arch Phys Med Rehabil. 2001;82(10):1407-11. https://doi.org/10.1053/apmr.2001.25992 PMid:11588745
Kolominsky-Rabas PL, Hiltz M, Neundoerfer B, Heuschmann PU. Impact of urinary incontinence after stroke: results from a prospective population-based stroke register. Neurourol Urodyn. 2003;22(4):322-7. https://doi.org/10.1002/nau.10114 PMid:12808707
Kohler M, Mayer H, Kesselring J, Saxer S. (Can) Not talk about it - Urinary incontinence from the point of view of stroke survivors: a qualitative study. Scand J Caring Sci. 2018;32(1):371-9. https://doi.org/10.1111/scs.12471 PMid:28544132
Tuong NE, Klausner AP, Hampton LJ. A review of post-stroke urinary incontinence. Can J Urol. 2016;23(3):8265-70. PMid:27347618
Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, et al. Post-stroke dysphagia: A review and design considerations for future trials. Int J Stroke. 2016;11(4):399-411. https://doi.org/10.1177/1747493016639057 PMid:27006423
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756-63. https://doi.org/10.1161/01.STR.0000190056.76543.eb PMid:16269630
Martino R, Martin RE, Black S. Dysphagia after stroke and its management. CMAJ 2012;184(10):1127-8. https://doi.org/10.1503/cmaj.101659 PMid:22125328 PMCid:PMC3394815
Mourão AM, Almeida EO, Lemos SMA, Vicente LCC, Teixeira AL. Evolução da deglutição no pós-AVC agudo: estudo descritivo. Rev CEFAC 2016;18:417-25. https://doi.org/10.1590/1982-0216201618212315
Cai W, Mueller C, Li YJ, Shen WD, Stewart R. Post stroke depression and risk of stroke recurrence and mortality: A systematic review and meta-analysis. Aging Res Rev. 2019;50:102-9. https://doi.org/10.1016/j.arr.2019.01.013 PMid:30711712
Terroni L, Sobreiro MFM, Conforto AB, Adda CC, Guajardo VD, Lucia MCS, et al. Association among depression, cognitive impairment and executive dysfunction after stroke. Dement Neuropsychol. 2012;6(3):152-7. https://doi.org/10.1590/S1980-57642012DN06030007 PMid:29213789 PMCid:PMC5618962
Das J, Rajanikant GK. Post stroke depression: The sequelae of cerebral stroke. Neurosci Biobehav Rev. 2018;90:104-14. https://doi.org/10.1016/j.neubiorev.2018.04.005 PMid:29656030
Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bull World Health Organ. 2016;94(9):634-634A. https://doi.org/10.2471/BLT.16.181636 PMid:27708464 PMCid:PMC5034645